5 Must-Have Features to Look for in an Electronic Health Records (EHR) System
Discover the top five crucial features that every healthcare professional should look for in an Electronic Health Records (EHR) system to enhance patient care and streamline operations.
Introduction to Electronic Health Records (EHR) Systems
The healthcare industry has witnessed substantial technological advancements over the past few decades. Among these innovations, Electronic Health Records (EHR) systems have emerged as a pivotal tool, revolutionizing how medical information is managed, accessed, and utilized. EHR systems are comprehensive digital platforms designed to store patients' medical records, treatment plans, histories, and other vital information. This digitization of health records has contributed immensely to enhancing the quality of patient care and improving the efficiency of healthcare delivery.
EHR systems provide a unified repository of patient data, making it possible for healthcare professionals to access and share pertinent information without the need for cumbersome paperwork or physical files. This electronic access ensures that crucial health data is available at the point of care, facilitating informed clinical decisions and fostering increased coordination and collaboration among healthcare providers.
One of the most striking features of EHR systems is their ability to streamline various administrative processes. These systems automate a range of tasks, from scheduling appointments and billing to managing prescriptions and tracking patient outcomes. Such capabilities not only reduce the potential for errors but also significantly decrease the time spent on administrative duties, allowing healthcare professionals to devote more attention to patient care.
Furthermore, EHR systems are not merely repositories of static information. They hold the potential to integrate with various analytical tools and applications, offering healthcare providers insights into treatment effectiveness and patient outcomes. By analyzing aggregated data, healthcare facilities can identify trends, optimize treatment protocols, and ultimately offer more personalized care based on empirical evidence.
In an era where data exchange is crucial, the interoperability of EHR systems with other healthcare technologies ensures seamless integration with laboratory systems, imaging systems, and external health networks. Such interoperability enhances the collective ability of health organizations to respond efficiently to patient needs, reduces redundancy, and minimizes potential errors in patient care.
As healthcare systems continue to face mounting pressures, including rising patient expectations and stringent regulatory requirements, the demand for efficient EHR systems is set to grow. Technologies like no-code platforms are transforming EHR development, making it faster and more cost-effective than ever before. With such platforms, healthcare entities can rapidly develop, deploy, and scale customized EHR solutions that perfectly align with their operational needs.
In summary, EHR systems play a crucial role in the modern healthcare ecosystem. They enhance operational efficiencies, enable high-quality care, and cater to the evolving landscape of healthcare delivery. For healthcare providers considering implementing or upgrading their EHR systems, understanding and selecting the right features is paramount to leveraging their full potential.
Interoperability: A Critical Feature for EHR Systems
In the increasingly interconnected healthcare environment, interoperability has become a pivotal aspect of an effective Electronic Health Records (EHR) system. Interoperability refers to the capability of different systems, devices, or applications to connect, exchange data, and use the information to improve patient care. For healthcare providers, having an EHR that integrates seamlessly with various health information systems is not just a convenience; it’s a necessity.
The primary aim of interoperability in EHR systems is to enable healthcare professionals to access and share patient data across different platforms, ultimately streamlining the care continuum. Here's why interoperability is a critical feature to seek in any EHR system:
Enhancing Clinical Collaboration
Interoperability facilitates collaboration among healthcare professionals, regardless of their location. This collective approach ensures that multiple specialists, primary care physicians, and clinics can share critical patient information efficiently. For instance, a surgeon in one hospital can quickly access the complete medical history of a patient treated by a different specialist in another facility. This level of coordination helps in making informed decisions, reducing the risk of errors, and delivering comprehensive care.
Improving Patient Safety and Care Quality
When EHR systems are interoperable, they provide a holistic view of a patient’s medical history, including allergies, existing medications, and past procedures. This comprehensive data availability decreases the likelihood of prescribing errors, ensures accurate diagnoses, and leads to more personalized treatment plans. By having real-time access to vital patient information, healthcare providers can enhance care quality and ensure better safety standards.
Optimizing Healthcare Workflows
Interoperability in EHR systems streamlines workflows by minimizing redundant paperwork and manual data entry. Healthcare staff can access and update patient records in real time, reducing administrative burdens and letting them focus more on patient-centric tasks. Furthermore, an interoperable system eliminates the need for repetitive diagnostic tests, thereby saving time and reducing healthcare costs.
Facilitating Public Health and Research
Beyond immediate clinical benefits, interoperability contributes to broader public health initiatives by providing researchers with access to aggregated health data. This data is valuable for disease surveillance, identifying health trends, and boosting research efforts aimed at developing new treatments or preventive strategies. As EHR systems continue to evolve, their role in supporting robust public health frameworks becomes increasingly vital.
Streamlined Technology Management
Integrated systems simplify technology management within hospitals and clinics. With interoperable EHR platforms, IT departments benefit from streamlined data management, easier system upgrades, and reduced need for complex integrations. This leads to enhanced efficiency and cost savings in maintaining and managing health IT infrastructure.
In summary, prioritizing interoperability when selecting an EHR system prepares healthcare organizations for future innovations in medical care and technology. It builds the foundation necessary for delivering high-quality, coordinated, and efficient healthcare services in today’s fast-evolving medical ecosystem.
User-Friendly Interface for Healthcare Professionals
In the realm of Electronic Health Records (EHR) systems, the user interface plays a crucial role in ensuring that healthcare providers can perform their tasks with efficiency and precision. A user-friendly interface contributes significantly to the overall usability of an EHR system, impacting both the quality of patient care and the productivity of healthcare professionals. This section delves into the key components that make an interface efficient and approachable.
Intuitive Design
An EHR system must have a design that is easy to navigate, allowing healthcare professionals to access patient data without confusion. An intuitive design ensures that essential features are easily accessible and that workflows mimic the natural thought process of healthcare providers. This reduces the time spent on data entry and retrieval, allowing professionals to focus on patient care.
Streamlined Workflows
Healthcare professionals deal with a range of tasks daily, from scheduling appointments to documenting treatment plans. A well-designed EHR interface integrates these tasks into a seamless workflow, reducing the need for multiple systems and minimizing the risk of errors. The ability to customize workflows within the EHR system can further enhance efficiency, catering to specific requirements of different departments or practices.
Enhanced Accessibility
An effective EHR system provides access on multiple devices such as desktops, tablets, and smartphones. Mobile compatibility ensures that healthcare providers can access critical patient information from any location, facilitating remote healthcare services and improving response times to patient needs.

Search and Filter Capabilities
The vast amount of data stored within an EHR system necessitates robust search and filtering functions. Comprehensive search tools allow healthcare professionals to quickly locate the patient records or specific data they need, thereby enhancing the speed and accuracy of decision-making. Filters help in narrowing down large datasets to display only the most relevant information, essential for managing patient care effectively.
Customizability
Each healthcare environment is unique, and the ability to customize the EHR interface to best meet the specific needs of a practice is invaluable. Customizable dashboards and field entry options can make the process more efficient, allowing for a more personalized and adaptable user experience.
Comprehensive Data Security Measures
The digitalization of healthcare records has brought immense benefits to patient care, but it also exposes sensitive information to potential cyber threats. Ensuring comprehensive data security measures is a fundamental requirement for any Electronic Health Records (EHR) system. Data breaches can have significant ramifications, including violations of privacy regulations, financial penalties, and loss of patient trust. Therefore, implementing robust security protocols is imperative to safeguard patient data.
Data Encryption
Data encryption is one of the primary defenses against unauthorized access. EHR systems should employ advanced encryption standards (AES) to protect data both in transit and at rest. This means that any patient information being transferred over networks or stored in databases is encoded in such a manner that only those with the correct decryption keys can access it. Encryption provides a layer of security that ensures even if data falls into the wrong hands, it remains inaccessible without the appropriate authorization.
Access Controls
Access control mechanisms are crucial for limiting who can view or manipulate sensitive patient data. Role-based access controls (RBAC) ensure that healthcare staff access only the specific data necessary for their role. Implementing multi-factor authentication (MFA) adds an additional layer of protection by requiring multiple forms of identification before access is granted, significantly lowering the risk of unauthorized entry.
Audit Trails
Maintaining a detailed log of all actions performed within the EHR system is essential for monitoring activities and identifying unauthorized or suspicious events. These audit trails provide a comprehensive record of who accessed what data and when, allowing healthcare organizations to track usage patterns and detect anomalies. Regular monitoring and analysis of this data help in proactively addressing potential security threats.
Compliance with Regulations
EHR systems must comply with various regulatory requirements such as the Health Insurance Portability and Accountability Act (HIPAA) and the General Data Protection Regulation (GDPR). Compliance ensures that data protection measures align with industry standards and legal obligations. Regular audits and assessments are necessary to verify ongoing compliance, adapt to evolving regulations, and implement improvements when needed.
Data Backup and Recovery
In the event of a security breach or system failure, the ability to restore data quickly and accurately is critical. Implementing a robust backup and recovery strategy ensures that patient information remains available and intact, minimizing data loss and disruption to healthcare services. Regular backups should be automated and secured to prevent tampering or unauthorized access.
Incorporating comprehensive data security measures into an EHR system not only protects sensitive information but also builds patient confidence in the healthcare provider’s technological competence. By prioritizing data integrity and security, healthcare organizations can deliver more reliable and trustworthy patient care.
Customizable and Scalable Solutions
When selecting an Electronic Health Records (EHR) system, customization and scalability are key factors that ensure the platform grows and adapts alongside the healthcare organization. An EHR system must cater to the unique needs and evolving demands of healthcare providers to deliver optimal efficiency and personalized care.
Customization: Tailoring the System to Fit Unique Requirements
Customization within an EHR system allows healthcare professionals to mold the software to meet specific organizational requirements and workflows. This flexibility is crucial for enhancing user experience and improving overall operational efficiency. Customizable EHR systems enable providers to adjust settings, features, and even the interface itself to align with their preferred methods of patient data management.
In particular, customization options can include:
- Interface Adjustments: Users can rearrange dashboards and personalize their data view for quick access to frequently referenced information.
- Modular Features: Healthcare facilities can integrate additional modules, whether they need specialized templates for ophthalmology, pediatric care, or any other focus area.
- Data Input Fields: Users can create and modify data fields to best capture and categorize essential patient information, aligning with the practice's specific data requirements.
Customization ensures that healthcare providers can design the EHR experience that best suits their practice's demands, ultimately improving workflow and minimizing the potential for human error.
Scalability: Adapting to Growth and Technological Advancements
Scalability in an EHR system refers to its ability to accommodate growth and technological advancements within the healthcare organization. As patient volumes expand or new services are introduced, a scalable EHR system should seamlessly adapt without compromising performance or data integrity.
Scalable solutions offer the following benefits:
- Capacity to Handle Increased Data: Systems should efficiently manage larger volumes of patient data, ensuring that analytics and decision-making processes remain accurate and timely.
- Seamless Integration of New Technologies: As telehealth, mobile health applications, and remote monitoring solutions become more prevalent, scalable EHR systems should easily integrate with these technologies to support comprehensive care delivery.
- Flexible Licensing & Resources: Scalable EHR systems should offer flexible licensing to accommodate varying sizes of practices, allowing healthcare providers to adjust resources as necessary without major disruptions.
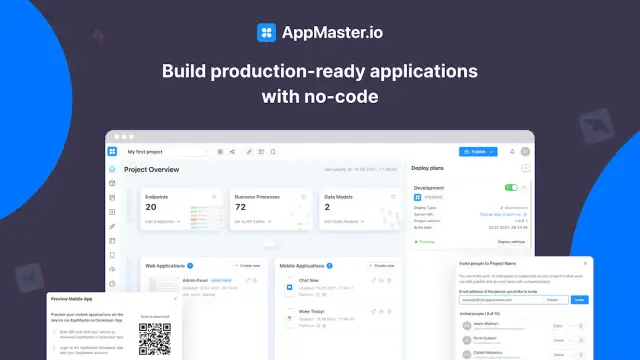
Leverage No-Code Platforms Like AppMaster
No-code platforms such as AppMaster have revolutionized the way customizable and scalable EHR systems are developed. By enabling healthcare organizations to quickly create, modify, and expand their EHR systems without extensive coding expertise, AppMaster significantly reduces costs associated with traditional software development.
AppMaster facilitates the creation of tailored, scalable EHR systems by providing tools that allow easy adjustments to data models and business processes via a visual editor. As healthcare providers adapt to new regulations, integration requirements, and patient care models, this no-code app builder helps them stay ahead of technological changes by offering continuous adaptability and growth potential.
In summary, a customizable and scalable EHR system is integral to modern healthcare operations. By offering flexibility to meet specific organizational needs and the ability to grow alongside advancements, such systems enhance efficiency and ensure that healthcare providers can continue delivering high-quality care.
Integration with Telehealth and Remote Monitoring
The increasing demand for telehealth and remote monitoring capabilities in the healthcare sector underscores the importance of integrating these functionalities into Electronic Health Records (EHR) systems. Having a seamless connection between EHRs and telehealth services is now essential for providing comprehensive patient care beyond the conventional confines of a healthcare facility.
Enhanced Patient Engagement
Integrating telehealth with EHR systems enhances patient engagement by providing easier access to healthcare services. Patients can consult with their healthcare providers without being physically present, making healthcare more accessible, especially for those living in remote areas or with mobility issues. This integration allows for the scheduling of virtual visits directly through the EHR system, enabling patients to manage appointments conveniently and receive timely care.
Real-Time Data Exchange
Integration with telehealth ensures that data captured remotely is immediately synchronized with the patient's EHR, maintaining up-to-date information. This capability allows healthcare providers to make informed decisions based on the latest data, be it vital signs, lab results, or imaging reports. A seamless data exchange also helps in monitoring chronic conditions effectively and promptly addressing any changes in a patient’s health status.
Streamlined Workflows
Integrating telehealth services into EHR systems streamlines workflows by reducing the duplication of data entry and minimizing errors. Healthcare providers can perform a comprehensive analysis by accessing all necessary patient data from a single platform, facilitating clinical efficiency and reducing administrative burden. This integration also supports automated notifications for follow-ups and prescription refills, optimizing the overall healthcare process.
Facilitating Remote Monitoring
Telehealth integration goes hand-in-hand with remote monitoring technologies, enabling patients to share their health metrics with healthcare providers in real time. The continuous flow of data from wearable devices and home monitoring equipment is fed directly into the EHR system, making it possible for healthcare professionals to track trends, foresee potential health issues, and intervene quickly when necessary.
Regulatory Compliance and Security
When integrating telehealth with EHR systems, it is crucial to ensure compliance with regulatory standards such as HIPAA, which govern patient data's privacy and security. By employing secure data encryption methods and robust access controls, EHR systems can protect sensitive information exchanged during telehealth sessions, thus building trust and ensuring compliance with industry standards.
FAQ
An EHR system is a digital platform that stores patients' medical history, treatment plans, and other healthcare data, accessible by authorized healthcare professionals.
Interoperability ensures seamless data exchange between different healthcare systems, enhancing clinical collaboration and improving patient care outcomes.
EHR systems must employ strong data security measures like encryption and access controls to protect sensitive patient information from unauthorized access and breaches.
A user-friendly interface in EHR systems boosts efficiency, reduces errors, and ensures a smooth user experience for healthcare professionals managing patient data.
Customization in EHR systems allows healthcare providers to tailor software functionality to meet specific needs, improving efficiency and adaptability.
Scalable EHR systems can grow with a healthcare organization, offering flexibility and resource adaptability to meet differing demands over time.
No-code platforms like AppMaster enable rapid development, customization, and deployment of EHR systems, significantly reducing time-to-market and development cost.
Yes, advanced EHR systems can seamlessly integrate with telehealth platforms, supporting remote patient monitoring and enhancing overall healthcare delivery.





