Why Interoperability in Electronic Health Records (EHR) Matters for a Connected Healthcare Ecosystem
Explore why interoperability in electronic health records is vital for a seamless, connected healthcare ecosystem, enhancing patient care and systems efficiency.

Introduction to Electronic Health Records
Electronic Health Records (EHR) have transformed the medical industry by digitally replacing traditional paper-based patient records. They serve as comprehensive and efficient means to collect, store, and share patient information across various healthcare settings. From a broader perspective, EHR systems are designed to facilitate coordinated, quality healthcare delivery by ensuring that critical patient data are readily available wherever and whenever needed.
The rising adoption of EHR systems is attributed to their capability to streamline and enhance healthcare operations, thereby contributing to improved patient outcomes. Unlike paper records, EHRs are not limited by physical boundaries; they can be securely accessed by authorized personnel from different locations, whether in hospitals, clinics, or other care facilities. This ubiquity ensures that healthcare providers have access to complete and up-to-date patient information, which is crucial for making informed decisions.
Furthermore, EHRs are instrumental in supporting public health initiatives by enabling the aggregation of large datasets and facilitating research and analyses. This data can assist in identifying healthcare trends, measuring patient care outcomes, and supporting evidence-based practices. As a result, EHRs are key enablers in elevating the overall standards of the healthcare ecosystem.
A vital feature of EHR systems is their ability to integrate with other healthcare technologies and systems, which is crucial for establishing a connected healthcare ecosystem. This integration capability allows seamless data sharing across various healthcare providers, fostering better communication and collaboration within the medical community. The drive towards a more interconnected and efficient healthcare system hinges on the successful implementation and operation of interoperable EHRs.
The Concept of EHR Interoperability
Electronic Health Records (EHR) interoperability is a vital cornerstone in the architecture of modern healthcare systems. It goes beyond merely having digital records for patients; it involves an integrated and well-communicated ecosystem where different EHR systems work harmoniously, sharing and utilizing patient information as required. But why exactly is this interoperability so crucial?
Interoperability in EHRs refers to the capability of different EHR systems to communicate, exchange, and interpret shared data effectively and reliably. Essentially, this means that patient information should be able to flow seamlessly between varied health systems, regardless of the software platform implementing each facility's EHR. In practice, a patient's medical history, current medications, allergies, or any other relevant medical data needs to travel with the patient across various care providers efficiently and accurately.
The significance of such interoperability lies in the promise of a cohesive healthcare experience that actively reduces the fragmentation of patient data. Effective interoperability can bridge the gap between disparate health systems, enabling healthcare providers to access essential information promptly and accurately. This accessibility can lead to more informed decision-making processes in patient care, significantly reducing the chances of errors such as incorrect prescriptions or redundant diagnostic tests.
For interoperability to work efficiently, it requires standardized data formats and protocols to ensure that all parties involved can understand and process the exchanged data similarly. This standardization simplifies the integration of different systems, fostering an ecosystem where patient data can be interpreted and utilized across various platforms and applications without unnecessary conversions or errors.
Beyond the technical aspect, EHR interoperability necessitates considerable collaboration among healthcare providers, software developers, and policymakers. This cooperation is essential to develop, implement, and enforce the necessary standards; it also promotes innovations that can make data exchange not only feasible but also secure and compliant with privacy regulations.
No-code tools contribute significantly to enhancing interoperability by empowering healthcare organizations to design and implement customized applications efficiently. These platforms simplify the back-end coding involved in integrating different systems, allowing for quicker adaptation to interoperability standards and the swift development of tailored solutions that meet specific healthcare needs.
Ultimately, EHR interoperability is a crucial step towards a more integrated and efficient healthcare system. It is about creating connections that matter, enabling healthcare providers to deliver high-quality, patient-centered care while maintaining systemic efficiencies and compliance. With the rapid advancements in healthcare technology, achieving genuine EHR interoperability may soon become less of a challenge and more of an opportunity to redefine healthcare interactions for the better.
Benefits of EHR Interoperability
The seamless exchange of patient information across various healthcare systems, known as Electronic Health Records (EHR) interoperability, brings a plethora of benefits to the healthcare ecosystem. This capability is crucial for enhancing the quality of care, improving patient outcomes, and increasing operational efficiencies. Let's explore these benefits in greater detail.
Enhanced Patient Care
Interoperability in EHR systems ensures that healthcare providers can access complete patient history from different sources, leading to more comprehensive and informed decision-making. Physicians and clinicians can offer better diagnoses and treatment plans, minimize errors, and avoid unnecessary tests by having real-time access to accurate patient data.
Improved Coordination Among Providers
When different healthcare providers can seamlessly exchange information, coordination among them improves significantly. This is particularly beneficial in cases where patients require multidisciplinary care involving multiple specialists. The ability to share updates efficiently ensures that everyone involved in a patient's care is on the same page, fostering better collaboration and consistency in treatment.
Reduction in Medical Errors
Access to accurate and up-to-date patient information is vital for minimizing medical errors. Interoperable EHR systems reduce the risk of medication errors, adverse drug interactions, and misdiagnoses by providing healthcare professionals with thorough insights into a patient’s medical history, allergies, and ongoing treatments.
Streamlined Workflow
Interoperability simplifies workflows within healthcare facilities by automating data transfer and integration processes. Automated systems save time that would otherwise be spent on manual data entry and retrieval, enabling healthcare professionals to focus on patient care instead of administrative tasks.
Cost Efficiency
Through reducing unnecessary medical tests and procedures, EHR interoperability leads to significant cost savings. It also cuts down on administrative costs tied to paper-based records and duplicated efforts. Additionally, by improving patient outcomes faster, healthcare systems can reduce long-term care costs.
Facilitated Research and Population Health Management
EHR interoperability supports public health by facilitating data collection for research and population health management. When data is readily accessible and shareable, it helps identify health trends, disease outbreaks, and efficiently allocate healthcare resources, ultimately contributing to better community health management.
Patient Empowerment
With interoperable EHR systems, patients have easier access to their health information, allowing them to take an active role in their healthcare management. They can quickly share their medical records with new healthcare providers, which is particularly beneficial for those who travel frequently or are relocating.
Overall, the benefits of EHR interoperability stretch wide and far, impacting not just patient treatment but also the operational and financial efficacy of healthcare services.
Challenges in Achieving EHR Interoperability
Interoperability in Electronic Health Records (EHR) is a crucial component of modern healthcare systems. However, achieving this seamless exchange of information is not without its challenges. Various barriers hinder the full realization of interoperability, causing healthcare systems to lag in efficiency and coordination. Here, we delve into the significant hurdles that organizations face when attempting to integrate EHR systems effectively.
Lack of Standardization
The absence of universally accepted standards for data formats and protocols is one of the central challenges in EHR interoperability. With healthcare providers and institutions using varied systems and software, the lack of standardization leads to compatibility issues. Different systems may store and classify data in unique ways, making it difficult to synchronize and interpret across platforms. This disparity necessitates the development of translators or interfaces, adding to the complexity and cost of interoperability efforts.
Data Privacy and Security Concerns
Safeguarding patient data is paramount in healthcare. Each exchange or integration of information increases the risk of data breaches or unauthorized access. Healthcare providers must comply with stringent regulations such as HIPAA in the United States, which ensure the protection of sensitive patient health information. Balancing ease of data exchange with robust security measures poses a significant challenge, often leading to reluctance in sharing information between systems.
High Implementation and Maintenance Costs
Financial constraints often impede the implementation of interoperable EHR systems. Developing and maintaining these systems requires substantial investments in technology and human resources. Small and rural healthcare providers, in particular, may struggle with the financial burden. These costs include purchasing new software, training staff, and redesigning existing processes to accommodate interoperable systems. In the absence of comprehensive funding or incentives, healthcare organizations may delay or avoid full-scale interoperability initiatives.
Resistance to Change
Resistance from healthcare staff and administrators can also be a challenging barrier. Established workflows and processes are deeply ingrained in the operations of healthcare facilities. Implementing interoperable solutions often requires significant changes to these workflows, leading to pushback from staff who may be resistant to adopting new technologies or methods. Educational programs and demonstrations of the benefits of EHR interoperability can aid in overcoming such resistance, but change management remains a critical hurdle.
System Compatibility Issues
Many healthcare systems have been developed as standalone solutions, resulting in a lack of compatibility with other systems. This siloed approach means that integration attempts often encounter difficulties in connecting disparate systems with varying architectures and interfaces. Creating middleware or other integration solutions to bridge these systems is a technical and logistical challenge that healthcare providers must address to enable true interoperability.
Fragmented Regulatory Requirements
Regulations governing EHR systems differ significantly across regions and countries. This fragmentation creates obstacles as healthcare providers operating in various locations must navigate a maze of legal and compliance requirements. International interoperability efforts face particularly tough challenges due to differences in data privacy laws, healthcare regulations, and administrative procedures, making it costly and time-consuming to implement cross-border data sharing solutions.
Addressing these challenges is essential for achieving effective EHR interoperability. Collaborative efforts among healthcare institutions, policy makers, and technology providers are necessary to overcome these hurdles. By bridging these gaps, we can pave the way for a more integrated healthcare system, ultimately leading to improved patient care and outcomes.
Solutions and Best Practices
Achieving interoperability in Electronic Health Records (EHR) is a crucial aspect of creating a connected healthcare ecosystem. While challenges exist, healthcare providers can adopt several solutions and best practices to enhance interoperability. Here are some strategic approaches:
Standardized Data Formats
One of the foundational steps towards EHR interoperability is the adoption of standardized data formats. Standards such as FHIR (Fast Healthcare Interoperability Resources) and HL7 (Health Level 7) provide a framework for the exchange, integration, sharing, and retrieval of electronic health information. By conforming to these standards, healthcare systems can ensure consistent and meaningful exchange of data across different platforms and providers.
Data Privacy and Security Compliance
Interoperability efforts must prioritize patient data privacy and security. Compliance with regulations like GDPR and HIPAA ensures that patients' sensitive information is protected during exchanges between EHR systems. Implementing robust encryption protocols and access controls are vital steps in safeguarding data and maintaining trust among patients and providers.
Comprehensive Stakeholder Collaboration
Achieving successful EHR interoperability requires collaboration among various stakeholders, including healthcare providers, technology vendors, and regulatory bodies. Stakeholders should work together to identify specific interoperability needs, share insights, and align goals. This collaborative approach can lead to more cohesive strategies and improve the overall effectiveness of interoperability initiatives.
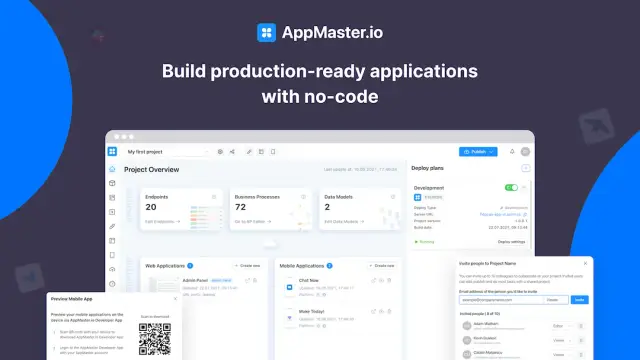
Leveraging No-Code Platforms
No-code platforms simplify the development of custom solutions that enhance EHR interoperability. These platforms enable healthcare providers to build and deploy applications without extensive coding knowledge. With visual interfaces for designing business logic and data models, such platforms can accelerate interoperability projects and reduce development costs.
Implementation of Integration Technologies
Integration technologies like API management and data integration solutions play a significant role in EHR interoperability. These technologies provide the necessary infrastructure for seamless data exchange and integration across disparate systems. API management tools help healthcare organizations manage data flows efficiently, ensuring secure and reliable connectivity among different EHR systems.
Continuous Training and Education
To foster a culture of interoperability, healthcare providers must invest in continuous training and education for their staff. Providing adequate training on new interoperable systems and designs helps reduce resistance to change and improves the overall adoption rate. Education efforts can also empower healthcare professionals to take full advantage of the benefits of interoperability.
Regular Assessment and Upgrades
Healthcare systems should conduct regular assessments of their EHR interoperability efforts. Evaluating the outcomes of interoperability initiatives can highlight areas for improvement and guide future investments. Additionally, staying updated on the latest technologies and advancements in EHR systems allows organizations to upgrade their solutions and maintain compatibility with evolving standards.
By focusing on these solutions and best practices, healthcare providers can effectively address the challenges of EHR interoperability and move towards a more connected and efficient healthcare ecosystem.
Technological Innovations in EHR Interoperability
The healthcare industry has increasingly recognized the need for electronic health records (EHR) interoperability to optimize patient care and resource allocation. As technology advances, innovative solutions are emerging, paving the way for seamless information integration across disparate systems. These innovations are poised to enhance EHR interoperability, significantly improving healthcare delivery.
Artificial Intelligence and Machine Learning
Artificial Intelligence (AI) and machine learning are revolutionizing how healthcare systems process and manage data. These technologies can analyze vast amounts of patient information, identify patterns, and provide actionable insights to healthcare providers. By leveraging AI algorithms, EHR systems can automatically map different data formats into standardized ones, thus promoting interoperability. Moreover, predictive analytics driven by machine learning can facilitate proactive patient care, transforming raw data into meaningful information.
Blockchain Technology
Blockchain technology has shown immense potential in enhancing data security and integrity, vital components of EHR interoperability. With its decentralized and immutable nature, blockchain can ensure that patient information is securely shared across multiple healthcare providers without compromising data integrity. This technology also allows for the efficient tracking of data exchanges, providing transparency and accountability in the process, thereby fostering trust among various entities in the healthcare ecosystem.
Internet of Things (IoT) Devices
The Internet of Things (IoT) is increasingly infiltrating the healthcare domain, offering new possibilities for EHR interoperability. IoT devices, such as wearable health monitors, continuously collect patient health data, which can be automatically updated into EHR systems. By enabling real-time data exchange, these devices play a crucial role in maintaining accurate and up-to-date patient records, ensuring that healthcare providers have immediate access to the latest information for making informed decisions.
Cloud Computing
Cloud computing has become an integral component of modern EHR systems, offering scalability, cost-efficiency, and enhanced accessibility. By hosting EHRs on cloud platforms, healthcare organizations can ensure that patient data is readily available to authorized personnel, facilitating seamless data sharing among different providers. Moreover, cloud-based solutions offer advanced security features, safeguarding sensitive health information and fostering a more interconnected healthcare environment.
API Standards and Open Platforms
Application Programming Interfaces (APIs) are crucial in enabling different software systems to communicate with each other. The development and adoption of standardized APIs, such as FHIR (Fast Healthcare Interoperability Resources), are pivotal in promoting EHR interoperability. These open platforms allow developers to create applications that can easily integrate with existing EHR systems, ensuring seamless data exchange across various healthcare service providers. The availability of open API protocols encourages innovation, allowing healthcare organizations to customize their solutions to specific needs.
By embracing these technological innovations, the healthcare industry can make significant strides toward achieving complete EHR interoperability. The integration of advanced technologies is driving a more connected and efficient healthcare ecosystem, ultimately benefiting patients and providers alike.
The Role of No-Code Platforms in EHR Integration
The digital transformation in healthcare is primarily fueled by the need for efficient data management systems, particularly concerning Electronic Health Records (EHR). The role of no-code platforms in enhancing EHR integration cannot be overstated, especially in an industry characterized by complex workflows and stringent regulatory requirements. These platforms eliminate traditional coding obstacles, allowing healthcare providers to focus on enhancing interoperability and improving patient outcomes.
Breaking Barriers in EHR Integration
No-code platforms significantly lower the entry barriers in the realm of EHR integration. They allow healthcare providers to develop and implement customized solutions without requiring extensive programming skills. This democratization of development fosters an environment where even professionals with minimal technical background can contribute to creating interoperable systems.
With features like visual data modeling and drag-and-drop interfaces, no-code platforms provide a user-friendly experience conducive to developing EHR integrations efficiently. These platforms support the rapid development cycle essential for healthcare environments that constantly evolve and require swift adaptation to new regulatory standards.
Customization and Flexibility
Customization is crucial when integrating EHR systems across different providers or departments. No-code platforms empower healthcare organizations by offering customization capabilities beyond what traditional coding practices can deliver in a timely manner. EHR systems can thus be tailored to specific workflows, enhancing operational efficiency and reducing the learning curve for employees.
No-code solutions enable healthcare providers to effortlessly adjust and update their EHR systems as new standards or needs arise. This flexibility ensures that the systems remain relevant and compliant over time, a critical aspect of maintaining robust healthcare operations.
Cost-Effectiveness and Efficiency
The cost-effectiveness of no-code platforms is a compelling reason for their growing adoption in healthcare. Traditional EHR integrations often involve substantial financial outlays in terms of hiring skilled developers and maintaining complex infrastructures. No-code platforms drastically cut these costs by offering a more straightforward, streamlined approach to building and managing applications.
The time efficiency is another significant benefit. Features like real-time collaboration and rapid prototyping allow teams to perform iterative testing and improvements, reducing the overall development timeline. As a result, no-code platforms enable faster deployment of EHR solutions that align with organizational goals.
Enhancing Interoperability with No-Code Solutions
Interoperability is at the core of effective EHR systems, driving seamless information exchange among diverse healthcare entities. No-code platforms inherently support interoperability by ensuring that the solutions developed adhere to established data standards and protocols.
AppMaster, for example, enables the creation of robust REST API and WSS endpoints, which are critical for facilitating communication between disparate systems. By allowing healthcare organizations to standardize and automate their data interactions, no-code platforms play a pivotal role in overcoming integration bottlenecks that have historically hindered EHR interoperability.
Future Outlook: Empowering Healthcare Innovation
As healthcare continues to evolve, the role of no-code platforms in EHR integration will likely expand. The flexibility, cost-effectiveness, and expedited development processes they offer align perfectly with healthcare's dynamic nature, positioning no-code as a key enabler of innovation.
By simplifying the integration of EHRs, no-code platforms pave the way for a more connected, efficient, and patient-centric healthcare ecosystem.
Future of EHR Interoperability
The future of Electronic Health Record (EHR) interoperability is poised for numerous advancements that promise to significantly enhance the healthcare ecosystem. As the demand for seamless information exchange continues to grow, healthcare systems are investing in technologies and practices that promise to fulfill this need while also ensuring patient privacy and data security.
Adoption of Global Standards
A pivotal factor in the future of EHR interoperability will be the broader adoption of global standards for health information exchange. Standards such as HL7, FHIR, and DICOM facilitate a common language for data sharing, ensuring that diverse healthcare systems can communicate effectively. The integration of these standards is expected to reduce discrepancies and ensure that patient data remains consistent and accurate across all digital platforms.
Role of Advanced Technologies
Emerging technologies like artificial intelligence (AI), machine learning, and blockchain are set to transform EHR interoperability. AI and machine learning algorithms can process vast amounts of health data, identifying patterns and generating actionable insights that improve patient care. Meanwhile, blockchain technology promises a decentralized approach to data security, offering enhanced protection against breaches and unauthorized data access.
Additionally, the integration of Internet of Things (IoT) devices is likely to further EHR interoperability. IoT devices, ranging from fitness trackers to smart implants, continuously generate patient data. Effective integration of this data into EHR systems will ensure that healthcare providers have comprehensive, real-time patient information, enabling more precise diagnoses and personalized treatment plans.
No-Code and Low-Code Platforms
No-code and low-code platforms like are gaining traction in the healthcare sector by simplifying the development process of EHR systems. These platforms enable the creation of customizable applications that can address specific interoperability challenges without requiring extensive programming knowledge. By empowering healthcare institutions to tailor their EHR solutions, these platforms ensure that interoperability can be achieved more quickly and cost-effectively.
No-code solutions offer an agile approach to development, accommodating the dynamic needs of modern healthcare environments. They facilitate rapid prototyping and implementation, allowing healthcare providers to respond swiftly to regulatory changes or emerging EHR standards.
Patient-Centric EHR Systems
The future of EHR interoperability is inherently patient-centric, with a focus on improving patient engagement and ownership of health data. As interoperability improves, patients will likely have more direct access to their medical records, enabling them to participate actively in their healthcare management. This empowerment fosters improved patient-doctor interactions and ultimately leads to better health outcomes.
Furthermore, patient portals and mobile applications are expected to become commonplace, delivering secure, user-friendly interfaces for accessing health information. By championing transparency and ease of access, these tools can enhance patient satisfaction and trust in healthcare services.
Collaboration and Policy Changes
Collaboration between stakeholders, including government bodies, healthcare providers, technology companies, and patients, will be critical in shaping the future of EHR interoperability. Policy changes that promote data sharing while safeguarding patient privacy will be instrumental in driving interoperability advancements. Governments and regulatory bodies worldwide are recognizing the necessity of cohesive policies that account for the complexities of health data exchange.
Ultimately, the future of EHR interoperability will rely on collective efforts to achieve a connected healthcare ecosystem. This connectedness has the potential to optimize healthcare delivery, reduce costs, and improve patient care quality on a global scale. As technologies continue to evolve and stakeholders commit to shared goals, EHR interoperability will become a cornerstone of a more efficient, patient-centered healthcare system.
FAQ
EHR interoperability refers to the ability of electronic health records systems to communicate and exchange patient information seamlessly across different platforms and healthcare providers.
Interoperability enhances the efficiency and quality of patient care by enabling seamless information sharing across different healthcare systems, thus improving decision-making and reducing errors.
Challenges include data privacy concerns, lack of standardized data formats, high implementation costs, and resistance to change from healthcare providers.
It allows for more accurate and timely access to patient information, which can lead to better treatment plans, reduced duplication of tests, and improved patient outcomes.
Yes, no-code platforms like AppMaster can simplify the development process, allowing healthcare providers to create customized solutions that enhance EHR interoperability.
Adopting standardized data formats, ensuring data privacy compliance, collaborating between stakeholders, and using advanced technology solutions are best practices for achieving EHR interoperability.
Technologies such as AI, machine learning, and blockchain are driving advancements in EHR systems, making them more secure and efficient.
By reducing redundant procedures and streamlining processes, interoperability can lead to significant cost savings in the healthcare system.
The future is promising, with increasing adoption of standardized practices, improved technologies, and more acceptance of no-code and low-code development platforms.
Engaging healthcare professionals in the development process, demonstrating benefits, and providing adequate training can help overcome resistance to interoperability.





