Telemedicine Platforms and Their Role in Mental Health Services
Exploring telemedicine's profound influence on mental health services, its benefits, challenges, and the innovative role of no-code platforms in enhancing healthcare solutions.
Introduction to Telemedicine in Mental Health
As digital technology advances and integrates into various facets of our lives, the healthcare sector has been significantly impacted, especially in the realm of mental health services. One of the most remarkable innovations in this domain is telemedicine, a method that leverages electronic communication to deliver healthcare services remotely. Particularly in mental health, telemedicine has facilitated a paradigm shift in how services are provided and received, offering unprecedented access and convenience to patients who might otherwise face barriers to accessing care.
Telemedicine, in the context of mental health, refers to the use of video conferencing, phone calls, mobile apps, and other digital tools to provide psychiatric evaluations, therapy, counseling, and other mental health support services. This transformation not only broadens the reach of mental health services but also addresses several socio-economic and geographic constraints that many patients encounter. From rural communities with limited access to healthcare providers to individuals with mobility challenges or time constraints, telemedicine serves as a crucial bridge connecting patients with the help they need.
Moreover, the COVID-19 pandemic has further accelerated the adoption of telemedicine in mental health, highlighting its effectiveness in maintaining continuity of care during times of restrictions and lockdowns. It has facilitated the ongoing monitoring and support of individuals with mental health conditions while reducing the risk of viral transmission inherent in face-to-face consultations.
However, the journey towards integrating telemedicine into mental health services is not without challenges. There are hurdles related to technology access, privacy concerns, regulatory compliance, and the importance of maintaining a human touch in therapy sessions. These factors necessitate careful consideration and innovative solutions to enhance the efficacy and acceptance of telemedicine in delivering mental health services.
A crucial component in overcoming these challenges is the rise of no-code platforms. These platforms empower healthcare providers to develop tailored telemedicine applications without the need for coding expertise, ensuring that solutions are adaptable, secure, and user-friendly. This democratization of technology plays a critical role in enabling mental health professionals to focus on patient care while technology handles the backend complexities.
As we continue to explore and improve telemedicine solutions, the potential to reform and enhance mental health services through digital means remains vast. The integration of telemedicine into mental healthcare systems holds promise for a more inclusive, accessible, and efficient delivery of care, benefitting millions of people worldwide seeking support and treatment for mental health conditions.
Benefits of Telemedicine for Mental Health Services
Telemedicine has revolutionized access to mental health services, bringing a multitude of benefits to patients and healthcare providers alike. By leveraging digital technology, telemedicine transcends geographical barriers, making mental health care more accessible and efficient. Here's how telemedicine is enhancing mental health services:
Increased Accessibility
One of the most significant advantages of telemedicine in mental health is its ability to reach patients in remote or underserved areas. With the help of telehealth platforms, individuals who may have been previously unable to receive care due to geographical restrictions can now connect with mental health professionals from the comfort of their own homes. This offers an immediate and practical solution for those living in rural areas where mental health resources may be scarce.
Reduced Stigma
The perception of mental illness is evolving, yet stigma still persists. Telemedicine allows patients to seek assistance discreetly, resulting in increased engagement in necessary treatments without the fear of being judged. By enabling users to participate in therapy sessions from familiar environments, telemedicine reduces social stigma and promotes a more open dialogue about mental wellbeing.
Convenience and Flexibility
Telemedicine adds unparalleled convenience to the process of mental health treatment. Patients can schedule appointments more swiftly and flexibly, eliminating traditional in-office waiting times. This flexibility is especially beneficial for people balancing demanding work schedules or caregiving responsibilities, as they can receive care during breaks or from home, without sacrificing other commitments.
Cost-Effectiveness
By eliminating the need for physical visits, telemedicine reduces associated transportation costs and time investments for both patients and providers. It also allows clinicians to manage their time more effectively by potentially reducing overhead costs associated with maintaining a physical practice. Consequently, telemedicine makes mental health services more affordable for a broader audience.

Enhanced Continuity of Care
Continuity of care is crucial for effective mental health treatment. Telemedicine fosters a seamless continuation of care by allowing follow-up appointments and ongoing therapy sessions to be conducted with minimal disruption. This helps maintain therapeutic momentum, which is vital for patient progress.
Timely Access to Specialist Care
Patients requiring specialized mental health care can access the expertise of specialists more swiftly through telemedicine platforms. This is particularly important for conditions that need prompt intervention, such as severe anxiety, depression, or post-traumatic stress disorder (PTSD). Timely access to specialists through telemedicine can result in better outcomes for patients as they receive the appropriate care without delay.
Challenges in Telemedicine Adoption
The adoption of telemedicine in mental health services has undoubtedly brought significant benefits, yet it also presents a set of challenges that cannot be overlooked. These challenges need to be addressed to unlock the full potential of telehealth services, ensuring they are both effective and secure for the end-users. Here, we delve into some of the key challenges currently faced in this field.
Data Privacy and Security Concerns
The protection of personal health information is a top priority in healthcare. With telemedicine, sensitive data is transmitted over the internet, increasing the risk of unauthorized access and cyber-attacks. Compliance with regulations, such as HIPAA in the United States, is necessary, yet ensuring this compliance poses a challenge. Healthcare providers must invest in robust cybersecurity measures, including encryption, two-factor authentication, and secure data storage solutions to protect patient information.
Technology Accessibility and Digital Literacy
Telemedicine platforms often require a reliable internet connection and compatible devices, both of which may not be accessible to all patients, especially those in rural or underserved areas. Additionally, varying levels of digital literacy among both patients and healthcare providers can hinder effective use. Simplifying user interfaces, providing tech support, and offering training can help bridge this gap, ensuring that telemedicine benefits are evenly distributed across different demographics.
Maintaining Patient-Therapist Engagement
While telemedicine provides convenience, it can also detract from the personal touch experienced in face-to-face therapy sessions. Establishing a strong therapeutic alliance virtually can be challenging, as non-verbal cues and body language are not as discernible. Healthcare providers must develop skills specific to teletherapy, such as enhancing verbal communication techniques to compensate for the lack of physical presence. Integrating features such as video calls, secure messaging, and virtual reality guided meditations can enhance patient engagement.
Reimbursement and Regulatory Barriers
Insurance coverage and reimbursement policies for telemedicine services can be inconsistent, leading to uncertainty and financial challenges for providers. Moreover, regulatory differences across regions and countries can complicate streamlined service delivery. Advocating for favorable legislative changes and clearer guidelines regarding telehealth reimbursement and licensing is crucial for more universal adoption.
Technical Integration with Existing Systems
The integration of telemedicine platforms with existing healthcare IT systems, such as Electronic Health Records (EHRs), can be technically challenging. Compatibility issues and the need for seamless data transfer can impede workflow efficiency.
Addressing these challenges requires a multifaceted approach, involving technological advancements, policy reform, and ongoing education. By systematically tackling these obstacles, telemedicine can continue to advance, creating a more accessible and efficient pathway for mental health care delivery.
Role of No-Code Platforms in Telemedicine
The advent of no-code platforms has become a game-changer in the telemedicine industry, especially in mental health services. By democratizing the software development process, these platforms allow healthcare providers to craft sophisticated digital solutions without the steep learning curve associated with traditional programming. No-code platforms have become an essential tool for developing telemedicine applications, enabling a wider range of professionals to participate in the creation and management of digital health solutions.
Empowering Healthcare Providers
No-code platforms empower healthcare providers by allowing them to develop customized telemedicine solutions tailored to their specific needs. This adaptability is crucial in mental health services, where the requirements of patients and practitioners can vary significantly. By enabling the customization of applications, no-code platforms ensure that mental health professionals can deliver personalized and patient-centric services.
For instance, mental health practitioners can develop appointment scheduling features, patient data storage, secure communication channels, and even automated reminders without needing to write a single line of code. The user-friendly interfaces of no-code platforms facilitate swift modifications and updates, ensuring that the applications can dynamically evolve with the needs of their users.
Fostering Innovation and Experimentation
No-code platforms encourage innovation and experimentation by reducing the barriers to entry for application development. Healthcare providers can test new ideas, implement solutions in real-time, and adjust their strategies based on feedback and evolving patient needs. The iterative nature of development with no-code platforms means that mental health professionals can continually refine their services, fostering a culture of continuous improvement and innovation.
Ensuring Data Security and Compliance
Data security and compliance with regulatory standards are perennial concerns in telemedicine, particularly in the mental health sector. No-code platforms help address these concerns by offering integrated security features and compliance tools. These platforms ensure that applications are developed with robust security protocols, safeguarding patient data against breaches and ensuring compliance with regulations like HIPAA.
With no-code platforms, healthcare providers can build applications that incorporate end-to-end encryption, secure authentication methods, and regular data backups. These security measures are built into the platform's framework, ensuring that even developers without a background in cybersecurity can create safe and compliant applications.
AppMaster as a No-Code Solution in Telemedicine
The versatility of no-code platforms is exemplified by AppMaster, which is empowering healthcare providers to create full-scale telemedicine applications with ease. With AppMaster, practitioners can seamlessly develop backend, web, and mobile application components integral to telemedicine solutions.
AppMaster offers powerful features such as the ability to visually create data models, build comprehensive business logic, and establish REST API endpoints. This makes it the go-to platform for developing scalable and responsive telemedicine applications that cater to the diverse needs of mental health services. The platform's capability to update applications swiftly, without accruing technical debt, makes it a forward-looking choice for healthcare providers who need to adapt to rapidly changing service requirements.
Moreover, AppMaster's robust approach to data security and privacy supports healthcare providers in meeting stringent compliance requirements. By facilitating a secure development environment, AppMaster ensures that healthcare providers can focus on delivering quality mental health services without compromising on data privacy.
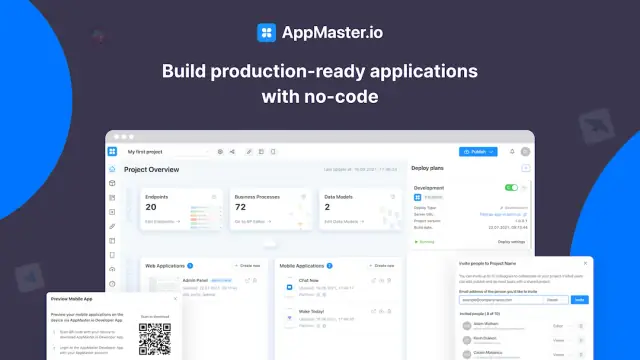
The role of no-code platforms in telemedicine is pivotal. By simplifying the development process, empowering healthcare providers, and ensuring robust security measures, no-code solutions are reshaping how mental health services are delivered.
Future of Telemedicine in Mental Health
Telemedicine's significant impact on the mental health sector has prompted a wave of interest, optimism, and innovation. As technology continues to evolve, the future of telemedicine in mental health is poised for remarkable advancements, ensuring that care is more accessible, efficient, and personalized than ever before.
Integration of Artificial Intelligence
Artificial intelligence (AI) is set to play a pivotal role in the future of telemedicine, particularly in mental health services. By leveraging AI, platforms can enhance diagnostic capabilities, provide personalized treatment recommendations, and support therapists by analyzing patient data more quickly and accurately. AI-powered chatbots, for instance, can offer immediate assistance to patients, facilitating triage, providing information, and enabling routine follow-ups, all of which ease the burden on mental health professionals.
Improved Data Security and Privacy
As telemedicine grows, so does the need for heightened data security and privacy measures. Future developments in this field will focus on ensuring robust encryption and data protection technologies to secure electronic patient records. The implementation of blockchain technology might become more widespread, offering a decentralized and tamper-proof way to handle sensitive mental health data, thereby improving trust and compliance among users.
Increased Accessibility and Inclusivity
The expansion of telemedicine technology promises to bridge existing gaps in mental health service accessibility. Future platforms aim to cater to underserved populations, such as individuals in remote areas or those with disabilities. Enhanced user interfaces and multilingual support are expected to make mental health services more inclusive and user-friendly, thus widening the reach of telemedicine and promoting mental wellness on a broader scale.
Blended Care Models
A significant trend in the future of mental health services will be the adoption of blended care models. These models combine in-person consultations with telemedicine, allowing for a more flexible and patient-centered approach to treatment. By integrating digital tools alongside traditional therapy methods, healthcare providers can offer a comprehensive suite of services tailored to individual needs.
Role of No-Code Platforms in Shaping the Future
No-code platforms are poised to revolutionize the development and deployment of telemedicine applications. These platforms enable healthcare providers, even those without technical expertise, to create bespoke mental health applications tailored to specific needs. By streamlining the application development process, no-code platforms ensure that innovative solutions can be rapidly designed, tested, and implemented, thereby accelerating the growth and evolution of telemedicine in mental health.
In summary, the future of telemedicine in mental health is bright, with many exciting technological advancements on the horizon. By incorporating AI, enhancing data security, expanding accessibility, and utilizing innovative platforms, mental health services will continue to evolve, ensuring better patient outcomes and broader access to care for everyone.
Conclusion
The integration of telemedicine into mental health services signifies a transformative epoch in ensuring accessible, equitable, and efficient patient care. This shift not only caters to the evolving demands of the modern healthcare landscape but also brings mental health interventions to the fingertips of those in remote or underserved areas. By overcoming geographical barriers and reducing the stigma often associated with seeking mental health care, telemedicine is pioneering a more inclusive future.
However, as with any technological evolution, the journey is not without challenges. Concerns over data privacy, access to technology, and maintaining the humane, empathetic connection critical to therapeutic relationships are concerns that must be tackled head-on. Education, continuous innovation in data security, and advancing digital literacy are stepping stones to overcome these hurdles.
The rise of no-code platforms plays a pivotal role in this transformation. These platforms democratize the field, allowing healthcare providers to rapidly develop, adapt, and deploy telemedicine applications tailored to their unique needs without the bottleneck of traditional software development processes. This agility ensures that mental health services can dynamically respond to patient needs and integrate the latest functionalities in mental health interventions.
As telemedicine continues to evolve, it heralds a future where mental health care becomes more accessible and personalized, fostering better health outcomes. Continued collaboration between healthcare professionals, technology providers, and policymakers will be essential to harness the full potential of telemedicine. Through joint efforts, we can ensure that mental health services are not only enhanced but also become a benchmark of quality, inclusivity, and effectiveness for generations to come.
FAQ
Telemedicine in mental health involves using digital platforms to provide mental health services remotely, improving accessibility and convenience for patients.
Telemedicine offers improved accessibility, reduced stigma, cost-effectiveness, and greater convenience for receiving mental health services.
Challenges include data privacy concerns, technology accessibility, and maintaining a satisfactory patient-therapist relationship remotely.
No-code platforms like AppMaster allow healthcare providers to easily create and manage telemedicine applications without traditional coding.
The future of telemedicine in mental health includes integrating AI, improving data security, and expanding accessibility to diverse populations.
While telemedicine offers numerous benefits, it is not a complete replacement for in-person therapy but can complement traditional services.
Telemedicine services implement various security measures like encryption to ensure patient data remains confidential and secure.
Telemedicine is vital for mental health as it helps overcome barriers to accessing care, including geographical, financial, and time constraints.
AppMaster offers no-code solutions that help healthcare providers develop and deploy telemedicine platforms efficiently, enhancing service delivery.
Several clinics and healthcare providers have successfully implemented telemedicine solutions, improving patient outcomes and service accessibility.





