Overcoming Barriers to Adopting Telemedicine Platforms in Your Practice
Explore strategies to overcome obstacles in adopting telemedicine platforms in healthcare practices, enhancing patient care, efficiency, and accessibility through digital technology.

Introduction to Telemedicine Platforms
Telemedicine, the application of digital technology to deliver healthcare services remotely, is reshaping the way medical professionals and patients interact. By utilizing electronic communications and information technologies, telemedicine allows for the exchange of medical information from one site to another, enhancing the healthcare experience by providing easy access to care, regardless of physical location. In a world where accessibility and convenience are paramount, telemedicine platforms are becoming indispensable tools for modern healthcare delivery.
These platforms, which vary in complexity from simple apps to sophisticated integrated systems, form the foundation for virtual consultations, diagnosis, and treatment. They facilitate real-time communication and collaboration between healthcare professionals and patients, reducing the need for in-person visits, which are often time-consuming and inconvenient.
The adoption of telemedicine platforms is accelerating due to increased demand for patient-centered care and a growing focus on improving healthcare accessibility. They offer a wide range of services, including medical consultations, remote monitoring, mental health support, chronic disease management, and post-operative follow-ups, among others. With the capability to deliver healthcare services efficiently to patients without physical barriers, telemedicine platforms have the potential to improve overall health outcomes and bridge gaps in healthcare delivery.
Despite their potential, the implementation of telemedicine platforms involves overcoming several hurdles, including technological, regulatory, and human factors. Healthcare providers need to understand these challenges and adapt their practices accordingly to fully harness the benefits of telemedicine. Additionally, leveraging modern solutions like no-code platforms can simplify the development and integration of custom telemedicine solutions tailored to specific practice needs.
As telemedicine continues to evolve, its integration into mainstream healthcare practices will likely transform the way care is delivered and experienced. By embracing telemedicine platforms, healthcare providers can ensure they remain at the forefront of this digital evolution, providing their patients with timely, convenient, and comprehensive care.
Understanding Barriers to Adoption
The integration of telemedicine platforms within healthcare practices promises vast benefits, yet significant challenges hinder widespread adoption. Understanding these barriers is crucial for developing strategies to effectively incorporate telemedicine into daily operations.
Technical Challenges
One of the most immediate barriers is the technological gap. Many healthcare practices lack the necessary infrastructure, such as high-speed internet or compatible devices, to support telemedicine effectively. Moreover, integrating telemedicine software with existing systems like Electronic Health Records (EHR) can present further complications.
Addressing these technical challenges often requires investing in new technologies and ensuring that IT systems are up-to-date and robust enough to handle the increased digital traffic that telemedicine demands.
Privacy and Security Concerns
Ensuring patient data safety is paramount in healthcare, presenting a significant barrier in telemedicine due to increased vulnerabilities like data breaches and unauthorized access. Regulatory requirements, such as HIPAA in the U.S., mandate stringent data protection measures. Adhering to these regulations necessitates investments in advanced encryption technologies and secure data management protocols.

Lack of Training and Awareness
Healthcare providers and staff may resist adopting telemedicine due to unfamiliarity with the technology or fear of disruption to established workflows. Comprehensive training programs are essential to equip personnel with the skills needed to operate telemedicine platforms effectively. Furthermore, demonstrating the benefits and efficiencies gained through telemedicine can help alleviate fears and encourage adoption.
Resistance to Change
Change management is a significant hurdle, as both providers and patients may prefer traditional, face-to-face interactions. Patients may be skeptical about the quality of care delivered through virtual consultations. This resistance can be mitigated by emphasizing the convenience, efficiency, and comparable quality of care that telemedicine provides, alongside clear communication about how these services work.
Regulatory and Compliance Issues
Navigating the regulatory landscape can be daunting, as telemedicine must comply with varying laws and standards across jurisdictions. These compliance requirements can delay implementation as practices work to ensure that all aspects are legally sound. Engaging with legal experts and utilizing compliance-support tools can ease this process.
In conclusion, overcoming these barriers requires a concerted effort from healthcare providers to invest in technology, train staff, and build patient trust.
Technical Challenges and Solutions
As healthcare practices transition towards digital platforms, technical challenges can pose significant hurdles in the adoption of telemedicine systems. These obstacles often include integration complexities, connectivity issues, and the need for robust IT infrastructure. However, with the right strategies and technologies, these challenges can be effectively overcome, enhancing the efficiency and reliability of telemedicine services.
Integration with Existing Systems
One of the primary technical challenges faced by healthcare providers is the integration of telemedicine platforms with existing electronic health record (EHR) systems and other healthcare IT solutions. A seamless integration ensures uninterrupted data flow, improves patient care, and enhances operational efficiency.
To address this, healthcare practices can leverage interoperable APIs (Application Programming Interfaces) designed to bridge the gap between disparate systems.
Enhancing Connectivity and Accessibility
Reliable internet connectivity is critical for the success of telemedicine services. Poor connectivity can lead to disruptions, causing inconvenience for both patients and healthcare providers. To mitigate this risk, practices should invest in high-speed internet solutions and consider redundant systems to ensure continuous service.
Moreover, telemedicine platforms should be accessible across various devices, including smartphones, tablets, and desktops, so that patients can connect with providers easily. This requires applications to be responsive and compatible with different operating systems and resolutions.
Establishing a Robust IT Infrastructure
The implementation of telemedicine demands a solid IT infrastructure that can support the storage and transmission of large volumes of sensitive medical data. This includes high-capacity servers, reliable data storage solutions, and advanced cybersecurity measures.
Healthcare practices can enhance their IT infrastructure by adopting cloud-based solutions, which offer scalability, flexibility, and cost-effectiveness. These solutions can handle increased demand and provide secure data storage and retrieval capabilities.
Implementing Cybersecurity Measures
Security concerns are paramount in telemedicine, where sensitive patient data is exchanged over digital platforms. Therefore, robust cybersecurity measures must be in place to safeguard against unauthorized access, breaches, and data leaks.
Healthcare practices should implement encryption protocols, multi-factor authentication, and regular security audits to safeguard data integrity. Utilizing platforms that automatically integrate these measures can vastly simplify compliance with healthcare data protection regulations.
In summary, by proactively addressing these technical challenges through strategic solutions, healthcare practices can successfully adopt telemedicine platforms and offer superior, uninterrupted patient care.
Addressing Privacy and Security Concerns
One of the primary concerns in adopting telemedicine platforms is ensuring the privacy and security of patient data. As healthcare providers integrate digital solutions into their practice, maintaining the confidentiality and integrity of sensitive information becomes a critical issue. Telemedicine's success hinges on effectively addressing these concerns, thereby building trust among patients and ensuring compliance with regulatory standards.
Understanding the Importance of Data Privacy
In the healthcare sector, patient data often contains highly sensitive information, including personal identifiers, medical histories, diagnoses, and treatment plans. The unauthorized access, use, or disclosure of such information can lead to severe consequences, including identity theft, breaches of confidentiality, and loss of patient trust. Therefore, healthcare providers must prioritize data privacy as an integral part of their telemedicine strategy.
Compliance with Healthcare Regulations
To address privacy and security concerns, healthcare providers must comply with established regulations and standards. In the United States, the Health Insurance Portability and Accountability Act (HIPAA) sets the standards for protecting patient data. Compliance involves implementing administrative, physical, and technical safeguards to ensure the confidentiality, integrity, and availability of electronic protected health information (ePHI).
Aside from HIPAA, international healthcare providers must also adhere to other relevant regulations such as the General Data Protection Regulation (GDPR) in the European Union. These regulations require strict control and monitoring of patient data, with substantial penalties for non-compliance.
Implementing Robust Security Measures
Healthcare practices adopting telemedicine must implement stringent security measures to protect patient data from cybersecurity threats. These measures may include:
- Data Encryption: Encrypting data both in transit and at rest to prevent unauthorized access during transmission and storage.
- User Authentication: Implementing multi-factor authentication (MFA) to ensure that only authorized users access sensitive systems and data.
- Access Controls: Restricting access to patient data to only those requiring it for direct patient care, thereby minimizing exposure to unnecessary personnel.
- Regular Audits and Monitoring: Conducting regular audits of the telemedicine systems to detect and address any potential vulnerabilities and unauthorized access attempts.
- Securing Communication Channels: Using secure communication tools for patient-provider interactions to prevent interception by unauthorized parties.
Training and Awareness Programs
A significant part of addressing privacy and security concerns involves educating staff on data protection practices. Regular training sessions should be conducted to inform healthcare professionals about the best practices for handling sensitive information within telemedicine platforms. Awareness programs should emphasize the importance of data security, breach reporting protocols, and the required actions to mitigate potential threats.
Conclusively, addressing privacy and security concerns is critical to the successful adoption of telemedicine platforms in healthcare practices. By ensuring compliance with regulations, implementing comprehensive security measures, and fostering a culture of data protection, healthcare providers can securely harness the benefits of telemedicine while maintaining the trust of their patients.
Training and Workforce Adaptation
The integration of telemedicine into healthcare practices necessitates not only a strategic overhaul of technology but also a pivotal shift in workforce dynamics. To ensure successful adoption, healthcare providers must proactively address the training and adaptation needs of their staff. This focus on education and skill development is crucial to fostering an environment where telemedicine can thrive.
Enhancing Technological Proficiency
A primary challenge in adopting telemedicine is bridging the technological gap among healthcare personnel. Many practitioners may lack the necessary skills to navigate digital platforms effectively. Providing comprehensive training sessions that cover both basic and advanced technological competencies ensures that all team members, regardless of their initial proficiency level, can operate telemedicine platforms with confidence. These sessions should include hands-on practice, simulations, and continuous learning opportunities to keep skills sharp.
Integrating Telemedicine into Clinical Practice
Healthcare providers must adapt their clinical workflows to incorporate telemedicine seamlessly. This integration requires retraining staff on new procedures that differ from traditional face-to-face interactions. By focusing on specific use cases, such as remote diagnostics and virtual consultations, training can help practitioners understand the nuances of digital patient engagements. Additionally, adapting to telemedicine involves rethinking appointment scheduling, billing practices, and patient follow-ups to accommodate virtual care delivery.
Building a Culture of Openness and Flexibility
Successfully integrating telemedicine into a healthcare practice demands a cultural shift towards openness and adaptability. Leadership must convey the importance of telemedicine and encourage the workforce to embrace change as a positive step towards modernization. By highlighting benefits — such as expanded patient reach and improved work-life balance for staff — organizations can ease potential resistance. Encouraging feedback and addressing concerns openly helps build trust and promote a culture receptive to technological advancements.
Promoting Collaboration and Multidisciplinary Teams
Telemedicine's adoption can be streamlined by fostering collaboration across multidisciplinary teams. Training programs should encourage team-based approaches, enabling healthcare practitioners to work cohesively within the digital space. Facilitating collaboration among physicians, IT specialists, administrative personnel, and other stakeholders ensures that each aspect of the telemedicine platform is well-coordinated and that there is ongoing support for all users.
Overcoming Resistance to Change
Resistance to new technologies is a common barrier in many industries, and healthcare is no exception. By actively involving staff in the decision-making process and providing a platform for open discussion, resistance can be minimized. Utilizing pilot programs to demonstrate telemedicine's effectiveness and gathering success stories from early adopters can motivate staff to overcome reservations.
The Role of Ongoing Support and Resources
A critical component in workforce adaptation is ensuring continuous support and access to resources. Implementing a robust support system, such as tech helpdesks or dedicated personnel for troubleshooting, guarantees that staff feel empowered to utilize telemedicine solutions confidently. Providing resources like training portals, user manuals, and online forums facilitates knowledge sharing and skill enhancement over time.
By investing in comprehensive training and fostering a culture that embraces digital innovation, healthcare practices can maximize the benefits of telemedicine.
Patient Engagement and Trust Building
One of the critical hurdles in the adoption of telemedicine platforms is ensuring patient engagement and the establishment of trust in these digital healthcare services. Patient engagement is pivotal because it directly influences the success of telemedicine by determining how effectively patients utilize these platforms for their healthcare needs. Trust, on the other hand, forms the foundation for sustained use and acceptance of telemedicine solutions.
Enhancing Communication and Transparency
To foster engagement and trust, healthcare providers must prioritize effective communication and transparency. This involves educating patients about how telemedicine works, its benefits, and addressing common concerns upfront. Clear instructions on accessing and using the platforms can help alleviate any apprehensions patients might have about the unfamiliarity with technology. Healthcare professionals should also be transparent about data usage and privacy policies to assure patients that their information is being handled securely and responsibly.
Delivering Personalized Patient Experiences
Personalization of healthcare services through telemedicine can significantly enhance patient engagement. Tailoring interactions to individual patient needs and preferences demonstrates that the provider values their unique health experiences. Utilizing patient data effectively to provide customized consultations and follow-ups can help build a stronger provider-patient relationship, increasing the likelihood of patient satisfaction and continued use of telemedicine.
Building Trust Through Reliability and Quality Care
Patients need to feel confident that they are receiving the same level of care through telemedicine as they would in face-to-face consultations. Ensuring high-quality interactions and demonstrating competence during virtual consultations can alleviate doubts about telemedicine's efficacy. Additionally, offering reliable and user-friendly platforms reduces frustrations and builds trust in the new modes of care delivery.
Addressing Patients' Privacy Concerns
One major concern that patients may have with telemedicine is privacy. Assuring patients of robust security measures for their personal and medical data is crucial. Providers can build trust by implementing and clearly communicating stringent data protection protocols and adopting platforms that prioritize patient privacy. Highlighting compliance with relevant privacy legislations such as HIPAA can further reassure patients of their data's safety.
Providing Continuous Support and Feedback Channels
Supportive, ongoing communication and feedback mechanisms play a significant role in maintaining patient engagement. Establishing accessible channels for patients to express concerns, ask questions, and provide feedback encourages a two-way engagement that can significantly enhance trust. Providers should be proactive in addressing patient feedback, which not only demonstrates caring, but also helps refine telemedicine services to better meet patient needs.
Regulatory and Compliance Considerations
As healthcare providers embrace telemedicine platforms, navigating the intricate web of regulations and compliance becomes a paramount concern. It's essential to address these considerations to ensure the legal and ethical provision of healthcare services while maintaining patient trust and safeguarding sensitive data. Here's an exploration of the primary regulatory challenges and how they can be mitigated.
Understanding Key Regulations
Healthcare providers must familiarize themselves with regulations at both the national and international levels. For instance, in the United States, the Health Insurance Portability and Accountability Act (HIPAA) governs patient privacy and data security. Meanwhile, the European Union has established the General Data Protection Regulation (GDPR), which impacts how healthcare providers operating in Europe must manage patient data.
These regulations demand that telemedicine platforms implement stringent data protection measures, secure patient consent for data usage, and establish transparent data handling protocols. Providers must stay updated on regulatory changes and adapt their practices to maintain compliance.
Licensure and Inter-State Practice
A significant regulatory challenge arises from the need for healthcare professionals to comply with licensing requirements across different jurisdictions. In many regions, including parts of the United States, medical practitioners must be licensed in the state where the patient is physically located. This can complicate the delivery of telemedicine services across state or national borders.
To address this, providers should explore licensure compacts and agreements that facilitate cross-border practice. Seeking legal counsel to navigate these intricacies can ensure adherence to licensure requirements while expanding the reach of telemedicine services.
Ensuring Data Security and Patient Privacy
The implementation of telemedicine platforms introduces additional concerns around data breaches and patient privacy violations. Healthcare providers must employ advanced security measures to protect patient information. This includes using end-to-end encryption, strong authentication protocols, and regular security audits to identify and address vulnerabilities.
Telemedicine Documentation Requirements
Proper documentation is a foundational component of compliance when adopting telemedicine platforms. Healthcare providers must meticulously record all telemedicine interactions, including session details, diagnosis, treatment plans, and prescriptions, in alignment with regulatory standards.
This documentation ensures that in the event of an audit or legal inquiry, providers can substantiate the care delivered. Adopting a standardized documentation process across all telemedicine interactions helps streamline compliance efforts and ensures consistency.
Strategies for Meeting Regulatory Challenges
To successfully maneuver through compliance challenges, healthcare providers can adopt several strategies:
- Conduct comprehensive compliance audits to identify potential areas of risk and address them proactively.
- Foster collaborations with regulatory experts who can provide specialized guidance and insights into evolving regulations.
- Invest in continuous education and training programs for staff, emphasizing the importance of compliance and its implications for patient care.
By understanding and addressing regulatory and compliance considerations, healthcare providers can confidently integrate telemedicine platforms into their practice, enhancing the quality and accessibility of care while maintaining trust and integrity with their patients.
Leveraging No-Code Platforms in Telemedicine
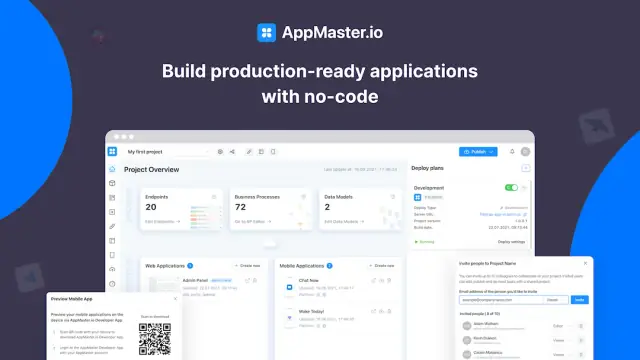
In the evolving domain of healthcare, the integration of telemedicine platforms has emerged as a pivotal innovation. With technological advancements reshaping medical practices, leveraging no-code platforms in telemedicine is proving to be a game-changer. These platforms eliminate the barriers traditionally associated with custom software development, making them indispensable for healthcare providers aiming to implement telemedicine solutions seamlessly.
The Power of No-Code Platforms
No-code platforms empower users by allowing them to create feature-rich applications without extensive programming knowledge. These platforms provide an intuitive drag-and-drop interface, enabling healthcare providers to design and deploy telemedicine applications tailored to their specific needs quickly.
One key advantage of no-code platforms is the speed at which applications can be developed and iterated. This agility is particularly beneficial in the healthcare sector, where rapid adaptation to emerging patient needs and regulatory changes is critical. With no-code solutions, healthcare organizations can focus on innovation, ensuring that their telemedicine offerings remain current and effective.
Customizing Telemedicine Solutions
Telemedicine requires a bespoke approach to meet the diverse needs of patients and practitioners. No-code platforms empower healthcare providers to customize their telemedicine solutions accordingly. Features such as appointment scheduling, secure patient communication, and electronic health record (EHR) integration can be easily incorporated and adjusted as necessary.
With platforms like AppMaster, healthcare providers can develop backend, web, and mobile applications that are fully interactive, ensuring a seamless user experience. The ability to create custom workflows and automate routine tasks can greatly enhance the efficiency of telemedicine services, freeing up medical staff to focus on patient care.
Enhancing Interoperability and Integration
No-code platforms offer robust integration capabilities, allowing telemedicine solutions to interact seamlessly with existing healthcare systems. This interoperability is crucial for maintaining comprehensive healthcare records and ensuring that patient data flows consistently across platforms. By integrating with existing EHR systems, telemedicine solutions can enhance continuity of care and improve clinical decision-making.
Moreover, the use of compiled applications ensures enhanced performance and scalability, accommodating the diverse needs of different healthcare organizations. The no-code approach also facilitates compliance with healthcare standards and regulations, addressing concerns pertaining to patient data security and privacy.
Cost-Effective Implementation
Cost is often a significant barrier in the adoption of new technologies within healthcare settings. No-code platforms substantially reduce development costs by minimizing the need for extensive coding expertise and resource allocation.
Scalability for Future Growth
Telemedicine is a dynamic field with evolving technologies and patient expectations. No-code platforms enable healthcare providers to scale their telemedicine offerings easily, adapting to increased demand or expanding service lines. As the needs of the healthcare environment continue to change, these platforms offer flexibility and scalability to support ongoing growth and transformation.
In conclusion, the integration of no-code platforms in telemedicine provides healthcare providers with a powerful tool for overcoming technological and operational barriers. By facilitating rapid application development and ensuring flexibility and cost-effectiveness, these platforms are redefining how telemedicine is delivered, ultimately enhancing patient care and practice efficiency.
Conclusion
Embracing telemedicine requires navigating a complex web of challenges and opportunities. By understanding and addressing the various barriers to adoption, healthcare providers can unlock the full potential of telemedicine platforms. From technical hurdles and privacy concerns to training needs and regulatory compliance, overcoming these obstacles paves the way for more accessible, efficient, and patient-centric care.
With the right approach, augmented by innovative solutions like no-code development platforms, healthcare practices can seamlessly integrate telemedicine into their services. This not only enhances their service offerings but also aligns with the broader goals of improved healthcare accessibility and patient satisfaction.
As the healthcare industry continues to evolve, telemedicine stands at the forefront of digital transformation, offering a pathway to more flexible and responsive care delivery. By effectively overcoming the barriers to adoption, healthcare practices can position themselves as leaders in technology-driven patient care, ensuring they meet the demands of the modern healthcare landscape and deliver optimal care to their patients.
FAQ
Telemedicine platforms are digital systems that facilitate remote medical consultations, diagnostics, and treatment, enabling healthcare providers to deliver care from a distance.
Telemedicine improves access to healthcare, especially for patients in remote areas, and enhances convenience for both practitioners and patients.
Common barriers include technical challenges, privacy concerns, lack of training, and resistance from both providers and patients.
By utilizing advanced technologies, such as no-code platforms like AppMaster, to simplify the development and integration of telemedicine solutions, these barriers can be mitigated.
Without proper measures, there is a risk of data breaches and patient privacy violations, making security an essential focus for adoption.
Effective training ensures that healthcare staff are equipped to use telemedicine platforms efficiently and can help decrease resistance to change.
Building patient trust through clear communication and demonstrating the benefits of telemedicine can help increase patient engagement.
Yes, compliance with healthcare regulations and privacy laws like HIPAA is crucial for legal and ethical telemedicine implementation.
No-code platforms, such as AppMaster, enable the quick creation and deployment of telemedicine applications without extensive coding, saving time and resources.
By investing in reliable technology and ensuring robust IT support, practices can overcome technical barriers to offer seamless telemedicine services.
Telemedicine enhances the accessibility and efficiency of patient care, offering timely consultations and continuous monitoring remotely.
Yes, telemedicine platforms can be seamlessly integrated with existing healthcare systems, improving overall practice efficiency and patient care. Tools like AppMaster can facilitate this integration.





