The Cost of Implementing Electronic Health Records (EHR): Is It Worth the Investment?
Discover the financial implications, benefits, and return on investment of implementing Electronic Health Records (EHR) systems in healthcare institutions.

Introduction to EHR Systems
Electronic Health Records (EHR) systems have revolutionized healthcare by digitalizing patient information, streamlining operations, and enhancing patient care. These comprehensive digital records go beyond simple patient charts; they integrate critical clinical and administrative data within a single, easily accessible platform. Collectively, EHR systems are designed to facilitate seamless communication among healthcare providers, ensuring that pertinent data is readily available when required, leading to more informed clinical decisions.
The transition from traditional paper-based systems to EHR is driven by the need for greater efficiency, improved accuracy, and better coordination among healthcare professionals. These systems empower clinicians by providing tools for electronic prescribing, test ordering, and accessible documentation of patient interactions. They also pave the way for improved patient engagement through patient portals, where individuals can access their own health data and communicate with their healthcare team directly.
Central to the promise of EHR is its capability to improve patient care outcomes. By maintaining comprehensive medical histories, tracking ongoing treatments, and enabling reminders for preventative health measures, EHR systems support proactive health management. The shift to electronic records can also enhance compliance with treatment guidelines and reduce medical errors by introducing decision support systems that alert practitioners to potential risks or contraindications.
Despite the clear advantages of EHR systems, their implementation is not without challenges. Healthcare institutions need to carefully weigh the costs, understand the necessary infrastructure, and plan for significant cultural shifts as staff adapt to new workflows. However, once integrated, the benefits of EHR systems typically justify their costs, particularly in the long term.
It's worth noting the role of innovative no-code tools, which have made the development and customization of EHR systems more accessible and cost-effective. By leveraging no-code solutions, healthcare providers can develop tailored applications to meet their unique needs without investing heavily in software development resources.
Understanding the Costs Involved in EHR Implementation
The decision to implement Electronic Health Record (EHR) systems comes with significant financial implications that healthcare providers must carefully consider. While the advantages of these systems are manifold, the initial and ongoing costs of adoption can vary widely. Understanding these costs is crucial to evaluate whether the benefits outweigh the expenditures.

Initial Costs
The initial costs of EHR implementation can be substantial and include several components. These upfront investments cover software licensing, where the choice between purchasing off-the-shelf solutions or developing custom EHR software can greatly influence expenses. Additionally, hardware costs involve upgrading or purchasing new computer systems, servers, and network equipment necessary to support the EHR infrastructure.
Another significant initial expense is implementation services. These entail the costs of consultants or developers who assist with the integration process, ensuring that the system meets the specific needs of the healthcare facility. This may also involve data migration from paper records or legacy systems, which requires precise planning and execution to avoid data loss or discrepancies.
Training Expenses
Training staff to effectively use the new EHR system is another critical expense. Comprehensive training programs are essential for successful adoption, requiring both time and financial resources. Healthcare providers must ensure that all employees, from administrative staff to practitioners, are adequately trained to utilize the system's functionalities, ensuring a smooth transition with minimal disruptions to daily operations.
Ongoing Maintenance and Support
Post-implementation, healthcare facilities incur ongoing costs for the maintenance and support of the EHR system. This includes software updates, IT support, security management, and regular system audits to ensure reliability and cybersecurity. Additionally, subscription fees for cloud-based EHR systems or data storage solutions can become recurring operational costs.
Hidden Costs
Aside from apparent costs, EHR implementation might lead to hidden expenses that are often overlooked. These can include productivity losses during the adjustment period as staff become accustomed to the new system. There is also a potential need for additional temporary staffing or overtime hours to manage workloads during the transition phase, further adding to the financial burden.
Given the range of costs associated with EHR systems, it's vital for healthcare providers to conduct a thorough financial analysis prior to adoption. This analysis helps assess the long-term benefits against the expenditures, ensuring that the investment in an EHR system will lead to improved efficiency, patient care, and ultimately, return on investment.
Benefits of EHR Systems for Healthcare Providers
The adoption of Electronic Health Records (EHR) systems in healthcare facilities presents numerous advantages that extend beyond the simple digitization of patient data. These systems are designed to refine clinical operations, enhance patient care, and facilitate better communication among healthcare workers. Here's a closer look at some vital benefits that EHR systems offer to healthcare providers:
Enhanced Patient Care and Safety
By making patient records easily accessible, EHR systems allow healthcare providers to access comprehensive patient histories, which helps in making informed decisions. This leads to reduced medical errors and increased accuracy in diagnosing and treating patients. With features such as alerts and reminders, EHR systems play a crucial role in preventing potential adverse events and drug interactions, thus enhancing patient safety.
Improved Coordination and Communication
Effective communication among healthcare team members is essential for delivering quality patient care. EHR systems facilitate seamless coordination by allowing various providers involved with a patient’s care to have real-time access to consistent and updated information. This aspect is particularly beneficial in complex cases requiring input from multiple specialists, ensuring all relevant data is synchronized and accessible.
Increased Efficiency and Productivity
The automation of routine tasks and elimination of unnecessary paperwork significantly increases the operational efficiency of healthcare providers. EHR systems streamline workflows and reduce the time spent on administrative tasks, allowing healthcare professionals to allocate more time to patient care. This efficiency results in increased productivity and improved patient throughput.
Comprehensive Data Management and Analysis
With the extensive data collection facilitated by EHR systems, healthcare providers gain the ability to compile and analyze patient data more effectively. This can lead to better healthcare outcomes by identifying patterns, trends, and risk factors, enabling providers to make data-driven decisions for preventative, personalized care.
Facilitated Compliance with Regulatory Standards
EHR systems are designed to assist healthcare providers in adhering to legal and regulatory standards. These systems assure compliance with healthcare regulations and standards such as HIPAA by implementing robust security measures to protect sensitive patient data. Automated audit trails in EHR systems further ensure data authenticity and transparency.
Cost Savings
Despite the initial investment required, EHR systems can lead to significant cost savings in the long run. The reduction of paperwork and elimination of redundant testing can lower operational expenses. Moreover, the increased accuracy in billing and coding can enhance revenue cycles by minimizing claim denials and optimizing reimbursement processes for healthcare providers.
While implementing EHR systems might seem a substantial undertaking, the benefits they provide in advancing healthcare delivery and practice efficiencies are undeniable.
Analyzing the Return on Investment for EHR Systems
When healthcare institutions consider implementing an Electronic Health Records (EHR) system, one critical factor in their decision-making process is evaluating the return on investment (ROI). Understanding both the financial performance and the qualitative benefits experienced over time can guide providers to determine if implementing an EHR system is a worthwhile investment. Let's delve into how ROI is analyzed in the context of EHR systems.
Cost Savings and Efficiency Gains
One major component of calculating ROI is assessing the cost savings and efficiency gains that an EHR system can bring to a healthcare practice. These systems can significantly reduce administrative burdens by automating mundane tasks, thereby cutting down on labor and operational costs. For instance, a decrease in time spent on managing paperwork and transcription processes allows staff to allocate their time to productivity-enhancing tasks.
With easy access to concise and accurate patient records, clinicians can make more informed decisions quickly, reducing unnecessary tests and treatments and minimizing medical errors. This not only improves patient outcomes but also generates financial savings for healthcare institutions by optimizing the resources utilized.
Revenue Enhancement Opportunities
In addition to cost reductions, EHR systems present opportunities to enhance revenue streams. Effective data management and streamlined billing processes can enhance the accuracy and completeness of billing, leading to faster claim submissions, reduced claim denials, and increased reimbursements from insurance providers.
Moreover, EHR systems facilitate better patient scheduling and management, increasing patient throughput and practice capacity. With optimized appointment scheduling, practices can avoid revenue loss from unbooked time slots while maintaining the same level of care quality.
Qualitative Benefits
While tangible financial metrics are easy to calculate, some of the greatest benefits of EHR systems are qualitative and may not be immediately quantified in financial terms. Enhanced patient safety, improved provider communication, and comprehensive reporting capabilities significantly contribute to long-term institutional value.
Patients experience better care coordination with EHR systems, leading to improved satisfaction and retention. Patient loyalty can drive revenue growth and act as a financial catalyst for healthcare institutions, attributable to successful EHR implementation.
Long-Term Value Creation
The long-term value EHR systems bring is pivotal in determining ROI. Beyond immediate cost savings and revenue enhancements, EHRs serve as an integral component for strategic growth and innovation. These systems support practices in compliance with evolving regulatory requirements, reducing the risk of penalties or legal issues that may affect financial stability.
Furthermore, by utilizing data-driven insights, healthcare providers can expand their service offerings, enhancing care quality and efficiency. This proactive approach facilitates the development of value-based care models that prioritize patient well-being.
Analyzing the ROI of EHR systems involves evaluating both financial performance and strategic benefits. While initial investment costs may be substantial, the promise of long-term savings, revenue enhancements, and qualitative improvements make EHR systems a prudent investment for many healthcare institutions.
Overcoming Challenges in EHR Implementation
The introduction of Electronic Health Records (EHR) systems in healthcare institutions promises significant improvements in patient care, data management, and operational efficiency. However, the journey to successful EHR implementation is not without its challenges. Addressing these difficulties is essential to reap the full benefits of digital transformation in the healthcare sector.
Initial Costs and Financial Concerns
The upfront investment for an EHR system can be a substantial barrier, especially for smaller healthcare practices with limited budgets. Costs include software, hardware, training, and ongoing maintenance. To overcome this, healthcare institutions often explore funding options such as government incentives, grants, and financial planning for phased implementation to spread costs over time.
Disruption of Operations and Workflow
Implementing an EHR system may cause temporary disruptions in daily operations as staff adjusts to new workflows and technologies. Healthcare organizations are encouraged to adopt a phased approach, starting with less critical areas and gradually expanding the system to minimize disruption. This also allows staff to get accustomed to the system in stages, reducing resistance to change.
Data Migration and Integration
Migrating existing patient records to the new digital format can be challenging, especially when dealing with large volumes of data. It often involves data cleansing and validation to ensure accuracy. Institutions must work closely with EHR vendors who have the expertise to handle data conversion and ensure seamless integration with existing health information systems.
Training and User Adoption
The success of EHR implementation heavily relies on effective training and user adoption. Healthcare providers must invest in comprehensive training programs tailored to different levels of technology proficiency within the team. Ongoing support and refresher courses are essential to ensure continuous improvement and adaptation.
Addressing Privacy and Security Concerns
Security is paramount when dealing with sensitive patient information. EHR systems must comply with stringent privacy regulations, such as HIPAA, to protect patient data. Choosing vendors with robust security protocols, regular audits, and data encryption can mitigate risks.
Addressing the challenges of EHR implementation requires strategic planning, the right technology partners, and an emphasis on continuous education and adaptability. With these in place, healthcare providers can successfully integrate EHR systems into their operations, ultimately leading to improved patient outcomes and business efficiencies.
The Role of No-Code Platforms in EHR Development
In recent years, the demand for efficient and customizable Electronic Health Records (EHR) systems has surged. EHR systems are critical in providing seamless and digitized patient information management. However, the conventional development of these systems can be encumbered by substantial costs, complex coding, and lengthy implementation periods. As such, the advent of no-code platforms is revolutionizing the way healthcare institutions approach the creation and deployment of EHR solutions.
Empowering Healthcare Providers
No-code platforms democratize the development process by enabling healthcare providers to create custom EHR applications without the need for specialized programming expertise. These platforms offer intuitive visual interfaces with drag-and-drop capabilities, allowing users to design applications tailored to their specific functional and operational needs. As a result, healthcare professionals can focus on enhancing patient care without being bogged down by technical development challenges.
Cost-Effectiveness and Efficiency
One of the primary advantages of utilizing no-code platforms is their ability to significantly reduce the cost and time involved in EHR development. By eliminating the need for extensive coding and minimizing the dependency on traditional software development teams, no-code tools lower the barriers to entry for small and mid-sized healthcare institutions. Moreover, these platforms expedite the development process, ensuring rapid deployment and enabling providers to quickly adapt to evolving healthcare needs.
Customization and Flexibility
No-code platforms provide unparalleled flexibility in customizing EHR systems to accommodate various healthcare workflows and specialties. With the ability to create bespoke solutions, healthcare institutions can ensure that their EHR systems integrate seamlessly with existing processes, thereby enhancing operational efficiency. The adaptability of no-code platforms also facilitates continuous improvements and updates, ensuring that EHR systems remain aligned with best practices and regulatory requirements.
Scalability for Growth
As healthcare organizations grow and evolve, their technological infrastructure must also scale accordingly. No-code platforms support scalability by allowing healthcare providers to effortlessly adjust their EHR systems based on changing requirements and expanding patient loads. This scalability ensures that institutions can maintain high levels of patient care and data management efficiency, regardless of organizational size or complexity.
Minimizing Technical Debt
No-code platforms effectively address the issue of technical debt by regenerating applications from scratch whenever changes are made to system blueprints. This feature eliminates the accumulation of outdated or inefficient code, a common challenge in traditional software development. By leveraging no-code platforms, healthcare providers can ensure that their EHR systems remain efficient, modern, and devoid of legacy code issues.
AppMaster as a Pioneering Solution
Among the leading no-code platforms, AppMaster stands out for its comprehensive feature set and user-friendly design. By supporting the visual creation of backend, web, and mobile applications, AppMaster empowers healthcare providers to develop fully interactive EHR systems that can be deployed across various platforms. With capabilities to generate source code and compile applications in real-time, AppMaster offers a seamless and efficient development experience. This makes it especially advantageous for healthcare institutions seeking to harness the power of EHR technology without being hindered by traditional development constraints.
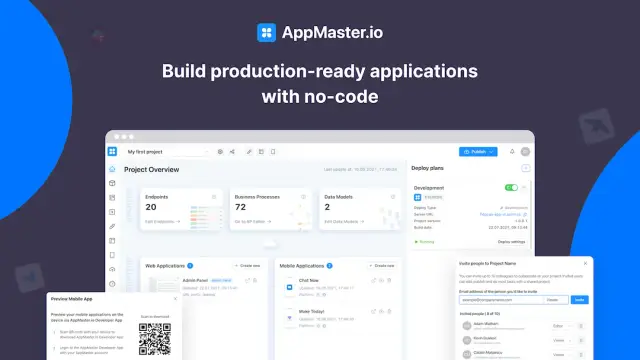
In conclusion, the role of no-code platforms in EHR development is transformative. By offering accessible, cost-effective, and customizable solutions, these platforms are empowering healthcare providers to innovate and enhance patient care delivery. As the healthcare industry continues to embrace digital transformation, no-code tools are set to play a pivotal role in shaping the future of EHR systems and healthcare technology as a whole.
Conclusion: Is EHR Worth the Investment?
The investment in Electronic Health Records (EHR) systems represents a significant expenditure for healthcare institutions, yet it comes with numerous profound benefits that justify the initial costs. At the forefront of these advantages is the enhancement of patient care. EHR systems provide healthcare practitioners with quick access to patients' comprehensive medical histories, leading to more informed decision-making and reducing the likelihood of medical errors. The improved accuracy and availability of records foster a higher quality of care, ensuring patients receive timely and effective treatments.
Moreover, EHR systems significantly optimize clinical workflows and operational efficiency. By digitizing patient records and automating routine administrative tasks, healthcare providers can direct more resources toward patient care rather than paperwork and logistical details. This increased efficiency translates into time and cost savings, enabling healthcare facilities to serve more patients and, consequently, increase revenue streams over time.
From a financial perspective, while the initial outlay for EHR implementations — covering software, hardware, and staff training — can be substantial, the long-term savings are hard to overstate. Reductions in transcription costs, fewer billing errors, and streamlined claim submissions can bolster financial performance, ensuring healthcare institutions improve their bottom lines over the years. Additionally, enhanced resource management enables facilities to better allocate assets and personnel, further driving cost-effectiveness.
The challenges associated with EHR system implementation, such as potential disruption during the transition period and the necessity of comprehensive staff training, are not insurmountable. Many healthcare organizations have successfully navigated these challenges by engaging with consultants and availing themselves of expert guidance, which strategically minimizes disruption and accelerates the learning curve for staff.
No-code platforms are reshaping the EHR landscape by providing healthcare providers with the tools to develop customized solutions swiftly. With no requirement for extensive programming, these platforms empower institutions, allowing them to craft EHR systems that precisely meet their operational needs and scale alongside technological advancements.
Considering all these factors, the investment in EHR systems goes beyond mere financial gains. The strategic implementation of EHRs translates into a healthier, more efficient, and forward-thinking healthcare environment. While clunning upward of costs might be intimidating at first, the holistic value offered through improved clinical outcomes, operational efficiency, and compliance with regulatory mandates makes EHR a worthwhile investment in the current and future landscape of healthcare.
FAQ
Electronic Health Records (EHR) are digital versions of a patient’s medical history, maintained over time, and include key administrative and clinical data.
Major costs include software and hardware expenses, implementation services, training for staff, data conversion, and ongoing maintenance and support.
EHR systems improve clinical workflows, enhance patient care, increase practice efficiency, enable better data sharing among practitioners, and ensure compliance with regulatory standards.
While initial costs can be high, EHR systems can result in long-term cost savings, increased revenue due to improved billing accuracy, and better resource management.
Challenges include high initial costs, disruption of practice operations during implementation, data migration difficulties, and the need for staff training.
No-code platforms, like AppMaster, streamline the development of EHR systems by allowing healthcare providers to create custom applications without extensive programming knowledge.
EHR systems automate clinical workflow, improve accuracy in patient records, and enhance communication among healthcare providers.
Popular EHR systems include Epic, Cerner, and Allscripts.
Implementation time can vary depending on the size of the practice and complexity of the system, but it typically ranges from a few months to a year.
Yes, EHR systems can be customized to meet the unique needs of different healthcare practices and specialties.
EHR systems help healthcare providers comply with legal requirements, such as HIPAA, by securely managing patient data.





