5 Common Challenges in Implementing Electronic Health Records (EHR) and How to Overcome Them
Explore common challenges in Electronic Health Records adoption and learn effective strategies to overcome them, ensuring a seamless digital healthcare transformation.

Introduction to EHR and its Importance
The healthcare sector is in the midst of a digital transformation, largely driven by the need for efficient, effective, and patient-centered care. At the heart of this transformation lies Electronic Health Records (EHR), which are rapidly becoming an integral part of the healthcare ecosystem. These digital records offer a comprehensive view of a patient's medical history, providing instant access to patient information and enabling smoother coordination among healthcare professionals.
EHR systems are replacing traditional paper-based records by capturing and storing comprehensive health information electronically. This shift addresses the limitations of paper records, such as accessibility, accuracy, and storage, enabling healthcare organizations to maintain a far more complete and accessible documentation system. By making patient information easily accessible to authorized users, EHR systems facilitate better-informed decision-making and improve the quality of care.
Beyond simply digitizing records, EHR systems offer numerous benefits, including improving clinical outcomes, enhancing patient safety, and increasing operational efficiencies. Patients benefit from these systems through improved management of their healthcare, receiving tailored treatment plans, and enhanced engagement in their long-term care. Healthcare providers gain the ability to speed up processes such as billing and reporting, reducing overheads and eliminating redundant paperwork.
However, the real value of EHR extends beyond internal efficiencies. These records are crucial for enabling interoperability across the healthcare system. As EHR systems are designed to communicate with different health information systems, they promote seamless data exchange across various platforms and organizations. This level of integration is vital in ensuring continuous and coordinated patient care, particularly in emergency scenarios where quick access to accurate medical histories can be life-saving.
Thus, in a world where connectivity and collaboration are paramount, the integration of electronic health records presents a significant advancement, transforming the healthcare industry and shaping the future of patient care.
Challenge 1: Data Migration and Conversion
Implementing an Electronic Health Record (EHR) system involves transferring vast amounts of historical medical data from paper records or older digital systems to a new, unified electronic platform. This data migration process is one of the most intricate and critical tasks in EHR implementation. The accuracy and completeness of this data significantly impact the quality of care provided and the overall success of the EHR system. However, several challenges can arise during data migration and conversion, making it a formidable obstacle for healthcare organizations.
1. The Challenge of Data Volume and Complexity
The sheer volume of data that needs to be migrated is a significant challenge. Medical records are comprehensive, including patient demographics, medical histories, diagnostic tests, treatment plans, billing information, and more. Moreover, the complexity increases when dealing with various formats and classifications used in different legacy systems, potentially leading to inconsistency and data loss if not handled carefully.
2. Ensuring Data Integrity
Maintaining data integrity throughout the migration process is crucial. Inconsistencies and errors during conversion can lead to incomplete or incorrect information, adversely affecting patient care and leading to legal liabilities. Ensuring that data is correctly mapped, verified, and validated before final migration is essential to uphold the integrity of patient records.
3. Addressing Compatibility Issues
Legacy systems often use proprietary formats that may not align with new EHR platforms, posing compatibility issues. Ensuring seamless integration requires developing custom solutions or employing middleware that can accurately convert and align the data structure between old and new systems.
4. Data Security and Compliance
During data migration, sensitive patient information is at an increased risk of breaches. Protecting this data through encryption, secure transfer protocols, and compliance with regulations such as HIPAA is critical. Failure to secure data can lead to severe repercussions, including legal penalties and loss of trust.

5. The Time and Resource Intensity
Data migration is time-consuming and resource-intensive, often requiring substantial personnel with expertise in data handling, IT, and healthcare operations. Allocating adequate resources and time for planning and execution is crucial to mitigate the risk of prolonged system downtimes and disruptions in healthcare delivery.
Solutions for Overcoming Data Migration Challenges
Addressing these complexities requires a strategic approach:
- Comprehensive Planning: Develop a detailed migration strategy that maps out each phase of the process, including risk assessment, timelines, and resource allocation.
- Data Mapping and Cleansing: Conduct thorough data mapping and cleansing before migration to ensure consistency and accuracy. Identify and rectify any discrepancies that may exist in legacy systems.
- Utilizing Automation Tools: Leverage automation tools designed to handle large datasets, identify patterns, automate repetitive tasks, and reduce manual errors.
- Engaging Skilled Personnel: Employ experienced IT professionals and data analysts who can navigate the technical challenges of data conversion.
- Implementing Security Measures: Use robust encryption and secure transfer protocols to protect sensitive data during migration, ensuring compliance with applicable regulations.
Challenge 2: User Training and Adaptation
The implementation of Electronic Health Records (EHR) systems is a significant milestone in the modernization of healthcare services. However, the transition presents a challenge often underestimated — user training and adaptation. It is not just about installing new software; it's about understanding and integrating an entirely new way of managing patient data and healthcare operations.
Why User Training is Crucial
Healthcare professionals, including doctors, nurses, and administrative staff, are the primary users of EHR systems. To ensure the successful adoption and efficient use of these systems, thorough training is indispensable. This training should cover all functionalities of the EHR platform that users will interact with during their daily tasks. The goal is to eliminate any resistance to change, which often stems from a lack of confidence or fear of the unknown regarding new technology.
Comprehensive training equips users with the necessary skills and knowledge to not only navigate the system but also to leverage its capabilities for enhanced decision-making and improved patient outcomes. Moreover, proper training helps in reducing errors, improving data accuracy, and increasing the overall efficiency of healthcare delivery processes.
Common Obstacles in Training
Several obstacles can hinder the effectiveness of EHR training. One of the primary challenges is the diverse familiarity with technology among healthcare workers. Some might be very tech-savvy, while others might only possess basic computer skills. This variation in tech comfort levels can slow down the training process and affect system utilization.
Another challenge is the resistance to change. Long-standing habits of recording data via paper have their inertia, and staff might see EHR systems as cumbersome. Healthcare professionals often have a busy schedule and may feel they cannot afford to invest substantial time in learning a new system, fearing it might initially slow them down.
Strategies for Effective Training and Adaptation
To address these challenges, a strategic approach to training is required:
- Tailored Training Programs: Develop programs that address different comfort levels with technology. Offering modular training that ranges from beginner to advanced can help cater to various learning paces.
- Role-Based Training: Customize training sessions according to the roles of the users in the healthcare setting. This ensures that specific and relevant functionalities of the EHR system are prioritized for each group, making the training more relevant and effective.
- On-the-Job Support: Provide continuous support post-training. Utilize super-users or digital champions within departments who are trained extensively to assist their colleagues, fostering a supportive learning environment.
- Feedback Mechanism: Implement routine feedback sessions to capture user experiences and rapidly address challenges they face with the system. Continuous improvement of the training process can be informed by these insights.
- Encourage a Learning Culture: Foster an organizational culture that values continuous learning and improvement, encouraging staff to view EHR as a beneficial tool rather than a burdensome obligation.
Transitioning to an EHR system, while transformative, requires concerted efforts in user training and adaptation. When executed effectively, it results in significant improvements in healthcare delivery and patient outcomes, paving the way for a digitized and more efficient healthcare future.
Challenge 3: Interoperability and Integration
The challenge of interoperability and integration in Electronic Health Records (EHR) is pervasive, affecting healthcare providers worldwide. Interoperability refers to the ability of different EHR systems, and other healthcare IT solutions, to communicate and exchange data effectively. Integration goes a step further, ensuring that these systems function seamlessly within an organization's existing technological ecosystem.
The Complexity of Interoperability in EHR Systems
Many healthcare institutions utilize varied systems to manage operations, from patient management systems to lab information systems. The sheer diversity of these applications poses a challenge when attempting to integrate and ensure smooth data flow across different platforms. The absence of standard data formats and protocols often results in fragmented healthcare delivery.
This challenge extends to EHR systems connecting with external entities, such as insurance providers, laboratory services, and pharmacy networks. Effective interoperability ensures that crucial information, such as patient history, medication details, and diagnosis reports, is available whenever required, irrespective of the specific system used.
Overcoming Interoperability Challenges
Addressing interoperability involves implementing standards and protocols that facilitate seamless communication between systems. Key strategies include:
- HL7 and FHIR Standards: Implementing standards like Health Level Seven (HL7) and Fast Healthcare Interoperability Resources (FHIR) provides frameworks that enable efficient data exchange.
- APIs and Middleware Solutions: Utilizing APIs (Application Programming Interfaces) and middleware solutions enables different systems to communicate more effectively by translating data formats and protocols.
- Collaboration with Vendors: Establishing strong partnerships with EHR vendors and other IT solution providers is crucial. Collaboration ensures that the solutions deployed work harmoniously and are updated as per evolving standards and requirements.
- Regulatory Compliance: Ensuring compliance with healthcare regulations aids in promoting standardization across systems, further facilitating interoperability.
In conclusion, while the challenges of interoperability and integration in EHR systems are significant, they can be effectively addressed with the right technological solutions, standardized protocols, and strategic collaboration. By fostering an environment of seamless data exchange, healthcare providers can ensure enhanced care delivery and operational efficiency.
Challenge 4: Privacy and Security Concerns
Privacy and security concerns are paramount when it comes to implementing Electronic Health Records (EHR) systems. In a healthcare setting, safeguarding sensitive patient information is not just a legal obligation but a moral one as well. Unauthorized access, data breaches, and cyber-attacks are significant threats that can undermine trust and compromise patient privacy. Understanding these risks and knowing how to mitigate them is crucial for any healthcare provider.
The Importance of Protecting Patient Data
Electronic Health Records contain troves of highly sensitive and personal information. From basic contact details to comprehensive medical histories, this information can be exploited if not adequately protected. A breach in an EHR system can result in identity theft, financial fraud, and other nefarious activities. Therefore, ensuring robust privacy and security measures is not just about compliance; it's about maintaining the integrity of the healthcare provider-patient relationship.
Common Security Threats in EHR
A myriad of security threats can target EHR systems:
- Malware Attacks: This includes viruses, worms, and ransomware that can infiltrate EHR systems, potentially leading to the encryption of patient data and demands for ransom.
- Phishing Attempts: Cybercriminals often use deceptive emails or messages to trick healthcare staff into divulging sensitive information, such as passwords or private encryption keys.
- Insider Threats: Employees with access to EHR systems can intentionally or unintentionally cause data breaches. This risk is heightened when access controls are lax.
- Weak Passwords: Simple or reused passwords make it easier for unauthorized users to gain access to EHR systems.
Mitigating Privacy and Security Risks
Addressing privacy and security concerns requires a holistic approach:
Implement Strong Access Controls
Use role-based access to ensure that only authorized personnel can access, modify, or input data into the EHR system. Regular audits should be conducted to verify that controls are in place and working effectively.
Regular Security Training
Conduct ongoing training sessions for healthcare staff about recognizing phishing attempts and the importance of secure password practices. Building a culture of security awareness is crucial.
Use Encryption
Encrypt both the data at rest and in transit to ensure that even if data is intercepted, it cannot be easily read or misused. Encryption acts as a crucial line of defense against unauthorized data access.
Conduct Regular Risk Assessments
Perform frequent assessments to identify vulnerabilities and potential risks. This proactive approach helps to mitigate threats before they can be exploited by malicious actors.
Ensure Compliance with Regulations
Adherence to regulations such as the Health Insurance Portability and Accountability Act (HIPAA) in the United States is vital. These regulations set the minimum standards for protecting health information and should be a foundational aspect of any EHR system.
Implementing these strategies not only protects sensitive patient information but also fortifies the credibility of healthcare institutions. With technology continuously evolving, staying ahead in terms of security and privacy measures is imperative for any modern healthcare provider.
Challenge 5: Cost and Resource Management
Implementing an Electronic Health Record (EHR) system is a significant undertaking that requires careful planning, particularly in managing costs and resources. The financial implications of integrating a new EHR system can be substantial, often causing concerns within healthcare organizations. Additionally, the allocation and optimization of resources for the successful deployment of EHR solutions present additional challenges.
Understanding the Cost Structure of EHR Implementation
The cost associated with EHR implementation is multi-dimensional, encompassing initial acquisition costs, ongoing maintenance, and support. Some of the primary cost factors include:
- Software Licensing Fees: The cost of purchasing software licenses for EHR systems can vary widely depending on the provider and the system's functionalities.
- Hardware and Infrastructure: Investments in hardware such as servers, workstations, and mobile devices, as well as networking infrastructure, are critical components that add to the initial expenditure.
- Installation and Customization: Customizing the EHR to meet specific organizational needs can be complex and expensive, often requiring technical expertise and time.
- Training and Support: Comprehensive training programs for staff are essential, adding to the cost, along with the necessity for ongoing support systems.
- Maintenance and Updates: Post-implementation costs include software updates, system maintenance, and potential scalability to support increasing data volumes.
Strategies for Effective Resource Management
Resource management is crucial to ensure that the implementation process is smooth and efficient. Several strategies can help in achieving effective resource allocation:
- Conduct Thorough Needs Assessment: Before selecting an EHR system, conduct a comprehensive assessment to understand the specific needs and capabilities of the organization. This process helps in choosing a solution that offers necessary functionalities without over-investing in unnecessary features.
- Phased Implementation Approach: Opting for a phased or incremental approach allows for the gradual allocation of resources and cost spreading over time, providing better control over the implementation process.
- Engage Stakeholders Early: Involving key stakeholders from various departments helps in identifying critical areas of concern that may require more resources, ensuring that the implementation aligns with operational goals.
- Optimize Training Programs: Investing in effective training programs is necessary, but optimizing these programs to be efficient, targeted, and adaptable can reduce costs while maintaining quality training standards.
- Leverage Cloud-Based Solutions: Utilizing cloud-based EHR solutions can reduce the need for extensive hardware and infrastructure, potentially lowering upfront costs and offering scalable solutions.
Leveraging No-Code Platforms for Cost Efficiency
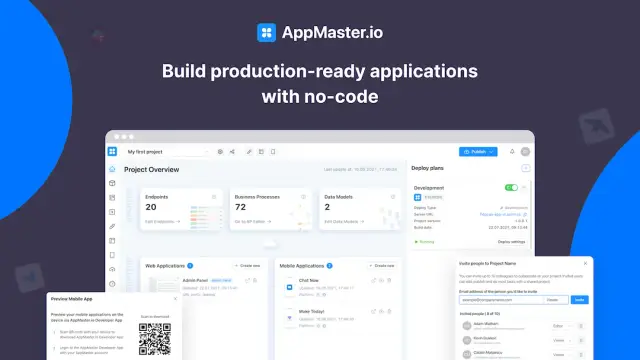
No-code platforms like AppMaster offer significant advantages in managing costs associated with EHR implementation. By enabling healthcare organizations to build custom applications without extensive coding expertise, no-code platforms simplify the development process, reducing the need for large development teams.
With AppMaster, healthcare institutions can quickly generate and deploy scalable solutions tailored to their specific needs, making the overall process more cost-effective. The platform's ability to automatically regenerate applications with each modification ensures that organizations can continuously adapt their EHR systems without incurring significant additional costs.
Ultimately, effective cost and resource management is indispensable to the successful implementation of EHR systems. By understanding the total cost of ownership, employing strategic resource allocation, and leveraging innovative solutions like no-code platforms, organizations can achieve a seamless transition to digital health records while maintaining financial stability.
Solutions and Best Practices
Successfully implementing Electronic Health Records (EHR) requires overcoming several significant challenges. By adopting thoughtful strategies and best practices, healthcare providers can ensure a smoother transition and maximize the benefits of digital records. Here are some ways to address these challenges effectively:
Comprehensive Data Assessment and Planning
Before migrating data from traditional paper charts or older systems to EHRs, it’s essential to conduct a complete data assessment and planning phase. Analyze existing data thoroughly, identify critical fields, and map them to the new system. Involving skilled IT professionals in this phase is crucial to ensure that data is accurate and aligns with the organization's needs. Extensive planning minimizes risks and supports a seamless migration process.
Investing in User Training and Support
One of the biggest hurdles in EHR implementation is user resistance due to lack of familiarity with new systems. Investing in comprehensive training for healthcare professionals is critical. Training sessions should cover all aspects of the system and be tailored to various roles within the healthcare facility. Ongoing support and refresher courses are also beneficial in helping users stay updated and confident in using the system.
Fostering Interoperability
To achieve efficient data exchange between different healthcare systems, prioritizing interoperability is essential. This can be accomplished by ensuring that the selected EHR system complies with set standards such as HL7 or FHIR, which streamline data integration across platforms.
Implementing Strong Security Measures
Addressing privacy and security concerns is a top priority when implementing EHR. Strengthen your system’s security by introducing access control measures, regular audits, encryption, and deploying token-based authentication. Adhering to compliance regulations such as HIPAA helps in maintaining trust and ensuring that patient data is protected from unauthorized access.
Working with Cost Management in Mind
Managing costs effectively is key to successful EHR implementation. Healthcare providers should adopt a phased approach, starting with the crucial components and integrating additional features as needed. This approach helps in spreading out costs and allows for adjustments based on user feedback.
Continuous Evaluation and Feedback
Continuous evaluation of EHR systems is essential to maintain efficiency and address emerging challenges. Collecting feedback from users, analyzing system performance, and making necessary adaptations ensures that the EHR continues to meet evolving clinical and operational needs. Regular evaluations help in pinpointing areas of improvement, promoting system efficiency, and ensuring that the EHR remains a vital tool for enhancing healthcare delivery.
By adhering to these best practices and leveraging modern solutions, healthcare facilities can foster a smooth transition to electronic health records and unlock their full potential. Such initiatives not only optimize patient care but also advance the healthcare sector's technological progress, leading to overall improvement in service delivery.
Conclusion
The implementation of Electronic Health Records (EHR) presents challenges that can be daunting if not properly addressed with strategic planning and execution. Despite the complexities surrounding data migration, user training, interoperability, privacy, security, and cost considerations, these challenges are not insurmountable.
Healthcare institutions must focus on adopting a systematic and structured approach to overcome the hurdles associated with digitizing patient records. By engaging key stakeholders, including IT professionals and healthcare staff, successful EHR implementation can transform the dynamics of patient care, streamlining operations and enhancing efficiency.
Ultimately, embracing potential barriers as opportunities for growth can foster a more robust healthcare environment. As technology continues to evolve, the seamless integration and implementation of EHR systems will be a cornerstone in achieving innovative and effective healthcare solutions, paving the way for improved patient outcomes.
FAQ
Electronic Health Records (EHRs) are digital versions of patients' paper charts. They provide real-time, patient-centered records that make information available instantly and securely to authorized users.
Implementing EHR systems can be complex due to issues like data migration, user training, interoperability, privacy concerns, and high costs.
Data migration challenges can be addressed by careful planning, data mapping, and using skilled personnel to ensure a smooth transition from paper to digital records.
User training is vital because without adequate training, healthcare professionals may struggle to adapt to the new system, leading to inefficiency and errors.
Interoperability refers to the ability of EHR systems to communicate and exchange data with other healthcare systems, ensuring a seamless flow of information.
Strengthening security protocols, using encryption, regular audits, and adhering to compliance regulations can help address privacy concerns in EHR systems.
EHR implementation involves initial costs, ongoing maintenance, and training expenses. Proper budgeting and choosing cost-effective solutions are crucial.
EHRs streamline access to patient information, enhance care coordination, improve diagnostic accuracy, and promote patient participation in healthcare management.
AppMaster can aid in creating custom, scalable applications essential for EHR systems, ensuring efficient and secure handling of health data.
Yes, EHR systems must adhere to various healthcare regulations such as HIPAA in the US, ensuring the protection of patient information.
Best practices include engaging stakeholders, thorough planning, phased implementation, comprehensive training, and continuous evaluation for improvements.





