Telemedicine Platforms vs. Traditional Healthcare: A Comparative Analysis
Explore the advantages and challenges of telemedicine platforms compared to traditional healthcare settings, and understand evolving patient care models.
Introduction to Telemedicine and Traditional Healthcare
As healthcare continues to evolve with the rapid advancements in technology, the emergence of telemedicine has initiated a fundamental shift in how patients access and receive care. Telemedicine, broadly defined, refers to the use of digital technologies to provide clinical services to patients without the need for an in-person visit. This method allows for the remote exchange of medical information via electronic communication channels, including video conferencing, mobile apps, and other online systems.
Traditional healthcare, on the other hand, has been the cornerstone of medical practice for centuries. It involves direct, face-to-face interactions between healthcare providers and patients, typically occurring in hospitals, clinics, or physician offices. This conventional model of healthcare allows for physical examinations, hands-on diagnostic processes, and in-person treatment delivery, factors which contribute to its longstanding reliability and trust among patients.
Both telemedicine and traditional healthcare offer unique benefits and limitations. Telemedicine provides easy access to healthcare services, particularly for individuals residing in remote or underserved areas. It enhances patient convenience by reducing travel time and wait times while also potentially lowering the overall costs associated with healthcare delivery. Conversely, traditional healthcare provides a tangible, personal touch to medical care, often forming the backbone of patient-provider relationships.
The integration of telemedicine within traditional healthcare systems presents an opportunity to complement the strengths of both approaches. As we navigate through the complexities of modern-day healthcare, understanding the intersection and interaction between telemedicine platforms and traditional healthcare methods becomes increasingly vital. In this analysis, we will delve deeper into the comparative aspects of telemedicine and traditional healthcare, exploring their benefits, limitations, and future potential in addressing the ever-changing needs of patients and healthcare providers alike.
Benefits of Telemedicine Platforms
The adoption of telemedicine platforms has seen a significant rise, driven by their range of benefits that address various challenges faced by traditional healthcare systems. Telemedicine utilizes technology to provide clinical health care from a distance, thereby transforming the way healthcare services are delivered. Let's explore some of the notable benefits that make telemedicine a compelling choice for healthcare providers and patients alike.
Increased Access to Healthcare
One of the primary advantages of telemedicine platforms is enhanced accessibility. These platforms allow patients living in remote or underserved areas to access quality healthcare services without the need to travel long distances. By bridging the geographic gap, telemedicine ensures that everyone has the opportunity to consult with healthcare professionals, regardless of their location. Particularly, individuals with limited mobility or those experiencing transportation barriers significantly benefit from telemedicine’s flexibility.
Convenient and Flexible Care
Telemedicine offers unparalleled convenience by providing healthcare services at the click of a button. Patients can schedule appointments at times that suit their busy schedules, eliminating the need to take time off work or school. For many, this flexibility translates into a better work-life balance and less stress associated with managing health care commitments. Real-time video consultations also enable patients to receive immediate medical attention when needed, preventing conditions from worsening due to delays in care.
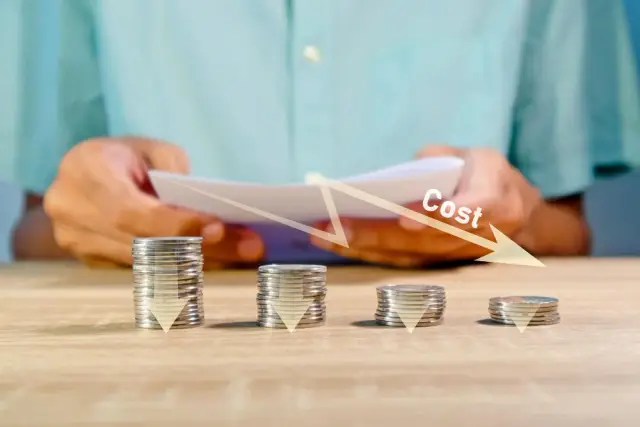
Cost-Effective Solutions
Telemedicine can help reduce healthcare costs for both patients and providers. Patients save on transportation expenses, childcare costs, and lost wages due to time taken off work. For healthcare providers, telemedicine reduces overhead costs associated with physical infrastructure, such as maintaining office spaces and staffing expenses. By optimizing resource utilization, telemedicine enables providers to increase their outreach and serve more patients efficiently.
Enhanced Continuity of Care
Continuity of care is critical for managing chronic conditions and ensuring patient safety. Telemedicine platforms facilitate consistent follow-up appointments, making it easier for patients to adhere to treatment plans and for providers to monitor ongoing health conditions. These platforms often integrate with electronic health records (EHRs), providing seamless access to patient data and histories, which in turn improves the quality and personalization of care.
Improved Patient Engagement
Telemedicine platforms enhance patient engagement by offering interactive and accessible healthcare experiences. Patients have greater agency in managing their health, as telemedicine empowers them with the tools to track their medical conditions, access educational resources, and communicate directly with their healthcare providers. This increased involvement can lead to better health outcomes, higher patient satisfaction, and stronger patient-provider relationships.
Reduction in Hospital Readmissions
By facilitating regular check-ins and timely interventions, telemedicine helps in reducing hospital readmissions. Patients recovering at home benefit from remote monitoring tools and virtual consultations that promptly address any arising issues post-discharge. This proactive approach ensures any complications are managed quickly, contributing to a smoother recovery process and reducing the likelihood of readmissions.
The benefits of telemedicine platforms position them as a powerful ally in modern healthcare services. By complementing traditional healthcare, telemedicine transforms patient experiences and opens new possibilities for innovative healthcare delivery models.
Advantages of Traditional Healthcare
Traditional healthcare remains a cornerstone of the medical industry due to its numerous inherent advantages. While telemedicine has expanded rapidly, the hands-on, personal nature of conventional healthcare cannot be overlooked. This section will delve into several benefits that traditional healthcare offers.
1. Comprehensive Physical Examination
One of the strongest arguments in favor of traditional healthcare is the ability to conduct a thorough physical examination. In-person visits allow healthcare professionals to perform precise diagnostic procedures such as palpating for abnormalities, auscultating heart and lung sounds, and conducting reflex tests. These procedures often provide insights that digital consultations cannot match, ensuring patients receive accurate diagnoses and effective treatment plans.
2. Personal Interaction
Traditional healthcare fosters an environment where personal interaction helps build trust and rapport between healthcare providers and patients. The importance of this cannot be underestimated, as a trusting relationship contributes significantly to patient comfort and cooperation during treatments. Personal interaction allows practitioners to notice subtle non-verbal cues and emotional expressions that might indicate additional concerns or conditions requiring attention.
3. Immediate Access to Comprehensive Testing
In a traditional healthcare setting, patients have immediate access to a wide range of medical tests and procedures, from blood tests and X-rays to advanced imaging techniques like MRIs and CT scans. This access allows for quicker diagnosis and the initiation of appropriate treatment plans, which can be crucial in emergency situations requiring urgent interventions.
4. Specialized Care and Referrals
Traditional healthcare settings are equipped with specialists who offer tailored expertise. In-person consultations facilitate smoother and more efficient referrals to specialists if complex conditions necessitate. The proximity of different specialists within the same facility or hospital often results in more cohesive patient care, ensuring that the patient receives the appropriate level of attention.
5. Supportive Network and Resources
Hospitals and traditional clinics provide a network of support and resources that enhance the overall patient experience. From immediate nursing care and pharmacy services to nutrition advice and counseling, patients receive a holistic treatment plan that addresses both immediate healthcare needs and long-term wellness goals.
6. Emergency Services
When emergencies arise, traditional healthcare facilities offer unmatched advantages. Quick access to emergency rooms, surgical teams, and critical care equipment is vital for saving lives and managing severe medical conditions. These services often require fast decision-making and advanced preparedness that digital platforms cannot adequately offer.
Ultimately, while telemedicine introduces unprecedented convenience and access, traditional healthcare maintains its status through capabilities that fully utilize hands-on methods, immediate testing options, and the advantageous personal engagement driving successful patient care. As technology continues to evolve, the synergy between traditional and digital healthcare modalities will likely transform patient experiences further.
Limitations and Challenges of Telemedicine
Telemedicine, while an innovative approach to delivering healthcare services, encounters several limitations and challenges that need to be addressed for optimal integration into the broader healthcare system. Despite its growing popularity, certain obstacles hinder its effectiveness and accessibility.
Technological Barriers
One of the most prominent challenges in telemedicine is the technological barrier. Patients and providers must have access to reliable internet connections and the necessary digital devices to participate in telehealth. In many rural and underserved areas, the lack of high-speed internet becomes a significant hurdle, limiting the reach of telemedicine services.
Additionally, the unfamiliarity with or reluctance to use new technology among certain patients, especially the elderly, can further impede the adoption of telemedicine. Comprehensive education and training programs can help bridge these gaps, but such initiatives require additional resources and planning.
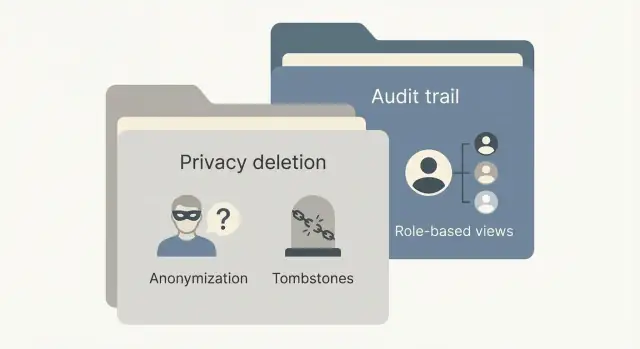
Privacy and Data Security Concerns
Privacy and data security are critical concerns with telemedicine platforms. Ensuring that patient information remains confidential and is protected against unauthorized access is essential. Telemedicine providers must comply with regulations such as the Health Insurance Portability and Accountability Act (HIPAA) to safeguard patient data.
However, with the increase in digital healthcare solutions, cybersecurity threats continue to evolve. Telemedicine platforms need to invest continuously in robust security measures to prevent data breaches and assure patients that their sensitive health information is secure.
Regulatory and Licensing Challenges
The legal and regulatory landscape for telemedicine remains complex and varies between regions. Healthcare providers must navigate a myriad of requirements related to delivering telehealth services, such as obtaining cross-state or international licenses where necessary.
Regulatory bodies need to standardize and simplify these processes to promote telemedicine's growth. Legislative advancements are required to support widespread adoption and to create a cohesive framework ensuring consistent standards across jurisdictions.
Scope Limitations
While telemedicine effectively manages numerous conditions and facilitates convenient access to healthcare providers, it cannot accommodate all medical scenarios. Certain diagnostic and treatment procedures require physical presence. For instance, conducting thorough physical examinations, emergency interventions, and specific medical imaging can't be achieved through telemedicine alone.
In these cases, telemedicine is often best used as a supplementary tool that complements in-person visits rather than replacing them entirely. Healthcare systems need to find a balance in integrating telemedicine into conventional practices to optimize patient outcomes.
Reimbursement and Cost Issues
The reimbursement structures for telemedicine are not always clear or equitable across different healthcare providers and insurers. In some cases, telemedicine consultations might not be reimbursed at the same rate as traditional in-office visits, which can discourage providers from offering these services.
Healthcare policies must evolve to offer fair compensation models that incentivize the use of telemedicine and recognize the value it provides in enhancing patient access and care continuity.
While telemedicine harbors several challenges, addressing these obstacles could significantly improve its integration into existing healthcare frameworks. For telemedicine to reach its full potential, technological, regulatory, and systemic changes are necessary to ensure its effective use as a comprehensive healthcare solution.
Adapting Traditional Healthcare to Modern Needs
In the past few years, the healthcare industry has witnessed tremendous shifts, fundamentally altering how care is delivered. With rapid advancements in technology and the evolving needs of patients, traditional healthcare systems must adapt to remain relevant and effective. This section delves into how healthcare systems are transforming and embracing modern needs by integrating digital solutions and innovative practices.
The Necessity of Integration
The integration of technology into traditional healthcare settings is no longer optional but rather a crucial necessity. Patients today are increasingly tech-savvy, demanding more accessible, convenient, and efficient healthcare services. In response, healthcare providers are adopting digital solutions to meet these expectations and enhance the quality of care.
Electronic Health Records (EHR) have become a standard component in maintaining patient data, improving the accuracy and speed of information sharing among healthcare professionals. This shift towards digital record-keeping allows for seamless integration and coordination of patient care across different medical departments, thus reducing the chances of errors and improving patient outcomes.
Enhancing Patient Engagement
One of the key aspects of modern healthcare is increasing patient engagement. Health systems are implementing patient portals and mobile apps that allow individuals to manage appointments, access medical records, and communicate effectively with healthcare providers. These platforms empower patients to take charge of their health, encouraging preventative care and contributing to better health management.
The use of telemedicine is a primary example of this shift. It not only enhances patient engagement but also bridges gaps, providing essential healthcare services to underserved populations in rural or remote areas. For instance, patients with chronic conditions can schedule virtual follow-ups with their doctors, making it feasible for them to receive consistent care without the need to travel.
Incorporating AI and Advanced Diagnostics
Artificial Intelligence (AI) plays a transformative role in reshaping traditional healthcare. By employing algorithms and predictive analytics, AI can efficiently analyze vast data sets to aid in early disease detection and personalized treatment plans. Advanced diagnostic tools powered by AI can provide more accurate results, thus enabling faster decision-making by healthcare professionals.
For example, AI-driven diagnostic imaging can interpret complex scans more accurately and faster than ever before, allowing for prompt action in critical care situations. Such innovations enhance the capacity of traditional healthcare systems to offer higher-quality patient care.
Addressing Regulatory and Ethical Concerns
As healthcare systems adapt to include more digital tools, regulatory and ethical challenges arise. Compliance with healthcare regulations, such as HIPAA in the United States, is necessary to ensure patient privacy and data security. Healthcare organizations must prioritize these considerations in their transition to digital solutions, instituting measures to protect sensitive patient information.
Furthermore, ethical dilemmas, such as keeping human oversight in AI-powered diagnostics, need to be considered to maintain trust and accountability in healthcare delivery. These concerns necessitate a balanced integration process, where digital tools complement rather than replace human expertise.
A Unified Vision for the Future
The integration of modern technologies into traditional healthcare models paves the way for an era of smarter, more responsive, and patient-centered healthcare solutions. By leveraging digital tools, healthcare systems can improve service delivery, enhance patient outcomes, and increase efficiency.
In conclusion, as healthcare evolves, traditional systems must embrace digital transformation to meet modern needs. By adapting, healthcare providers ensure that they deliver the best possible care while maintaining patient satisfaction in an ever-changing world.
Technological Influence in the Healthcare Revolution
The transformation of healthcare through technology is both remarkable and relentless. With the emergence of innovative tools and platforms, the healthcare industry is undergoing a revolution, building a bridge between traditional healthcare practices and future possibilities. One of the driving forces behind this evolution is telemedicine, a sector that has gained momentum in recent years due to advancements in digital communication technologies.
Emergence of Telemedicine Platforms
The advent of telemedicine platforms is a key testament to the technological revolution in healthcare. These platforms leverage high-speed internet and sophisticated software solutions to deliver healthcare services remotely. Patients can consult with healthcare providers from the comfort of their homes, eliminating geographical barriers and enhancing the overall patient experience. Telemedicine expands access to care for individuals residing in rural and underserved areas, offering a glimpse of how technology can democratize healthcare access.
Impact of Artificial Intelligence and Machine Learning
Artificial Intelligence (AI) and Machine Learning (ML) have introduced new dimensions to healthcare service delivery. AI algorithms are being used to predict patient outcomes, personalize medicine, and provide clinical decision support. Machine learning models analyze massive datasets to identify patterns and generate insights that were previously unattainable. From AI-driven diagnostic tools to predictive analytics, artificial intelligence is now a cornerstone of modern healthcare, augmenting the capabilities of healthcare providers.
Electronic Health Records and Digitalization
Electronic Health Records (EHRs) signify one of the most significant developments in medical records management. EHRs provide a centralized and digitized version of patient data, making it easier for healthcare professionals to access patient histories, track treatments, and coordinate care. The interoperability of EHR systems allows for the seamless exchange of information between healthcare providers, enhancing collaborative care and improving patient outcomes.
Role of No-Code Platforms
The role of no-code platforms in the healthcare technological revolution cannot be overstated. Platforms like AppMaster empower healthcare institutions by enabling them to develop custom healthcare applications swiftly and cost-effectively. With no-code platforms, healthcare providers can create tailored solutions for specific needs, such as patient management systems, telemedicine applications, and remote monitoring tools, without extensive programming skills. This democratization of software development allows smaller healthcare practices to innovate and stay competitive in the digital era.
Wearable Technology and Remote Monitoring
Wearable devices and remote monitoring technologies have gained traction, giving individuals the tools to monitor their health continuously. Wearables like smartwatches and fitness bands can track vital signs, physical activity, and even sleep patterns. Such devices play a pivotal role in preventative healthcare, encouraging individuals to take an active role in managing their health while allowing healthcare providers to monitor patients remotely.
Blockchain in Healthcare
Blockchain technology offers potential improvements in areas such as data security, transparency, and transaction integrity. In healthcare, blockchain holds great promise for securing digital health records, managing supply chains, and authenticating pharmaceuticals. The decentralized nature of blockchain technology can enhance data integrity, reduce fraud, and improve trust in healthcare systems.
The integration of technology in healthcare is a dynamic process, continually reshaping the way care is delivered and experienced. As telemedicine, AI, no-code platforms, and other innovations converge, the healthcare industry is on the brink of unprecedented transformations that promise a future where healthcare is accessible, personalized, and efficient.
Legal and Ethical Considerations
The evolving landscape of telemedicine brings a unique set of legal and ethical challenges that healthcare providers and platforms must navigate. As the digital transformation of healthcare accelerates, the emphasis on patient privacy, data protection, and cross-border healthcare delivery demands particular attention.
Patient Privacy and Data Protection
One of the most significant concerns regarding telemedicine is ensuring patient privacy and data protection. Healthcare providers must comply with stringent regulatory standards such as HIPAA in the United States or GDPR in the European Union to safeguard sensitive patient information. These regulations mandate that healthcare platforms implement strong security measures to prevent unauthorized access and breaches.
Telemedicine providers must ensure encrypted communication channels during consultations, secure data storage solutions, and robust authentication procedures. Compliance is not only a legal obligation but a crucial component of maintaining the trust and confidence of patients using telemedicine services.

Licensing and Interstate Practice
Another complexity involves medical licensing and the ability of healthcare professionals to practice across state or national borders. Many healthcare systems are regulated on a regional level, requiring practitioners to hold valid licenses in each jurisdiction where they offer telemedicine services. This presents a challenge for telemedicine platforms that aim to provide care over wide geographic areas.
Efforts to streamline licensing processes are underway, such as interstate licensure compacts that grant physicians the ability to operate across multiple states without the need for separate licenses. Telemedicine providers must stay informed about the licensing requirements and ensure compliance to legally serve patients in different regions.
Informed Consent
Informed consent remains a cornerstone of ethical medical practice, and telemedicine is no exception. Patients must clearly understand the nature of telemedicine services, the risks and benefits involved, and how their data will be handled. Providers are responsible for obtaining documented consent from patients before initiating telemedicine consultations.
Educating patients about their rights and the specifics of telemedicine can help facilitate informed decision-making, improving patient engagement and satisfaction with digital health services.
Quality of Care and Responsibility
Maintaining a high standard of care is a legal and ethical obligation for telemedicine practitioners. The responsibility lies with healthcare providers to ensure that remote consultations do not compromise patient safety or the quality of care.
Clinicians must be adequately trained in using telemedicine technologies, able to identify cases that require in-person evaluation, and document all telemedicine interactions thoroughly. Telemedicine should be integrated as part of a broader healthcare strategy, complementing — not replacing — face-to-face interactions where necessary.
Ultimately, the success of telemedicine platforms in addressing legal and ethical challenges will depend on continuous engagement with evolving regulations, proactive patient education, and commitment to quality care.
Conclusion: Future of Healthcare
The future of healthcare is poised at an intriguing and transformative crossroads, wherein the rapid advancement of technology will continue to reshape patient care and the broader medical ecosystem. Telemedicine stands at the forefront of this transformation, offering a preview of how healthcare delivery will evolve to meet the demands of a digitally-savvy patient population.
Integrated Technologies. As healthcare providers and patients become increasingly reliant on technology, the integration of telemedicine with other digital health solutions such as artificial intelligence (AI), machine learning, and wearable technology will significantly enhance diagnostic capabilities and treatment personalization. These technologies will not only improve patient outcomes but also provide healthcare professionals with powerful tools to make data-driven decisions.
Increased Accessibility. Telemedicine will continue to bridge the gap between healthcare access and underserved populations, bringing quality medical care to remote and rural areas. Its ability to break geographical barriers provides patients with access to specialists and tailored care plans regardless of location. As internet infrastructure and connectivity improve globally, this accessibility will only increase.
Regulatory Evolution. To fully capitalize on the benefits of telemedicine, regulatory frameworks will need to adapt in tandem with technological advancements. Governments and healthcare organizations must work together to establish standardized guidelines that prioritize patient safety, data protection, and cross-border practice, thus encouraging more widespread adoption of telemedicine solutions.
No-Code Solutions in Healthcare. No-code platforms will complement this evolution. By enabling healthcare providers to rapidly develop custom applications without extensive coding expertise, no-code solutions will help healthcare institutions streamline operational processes and enhance patient engagement through personalized digital interfaces.
The synergy between telemedicine, traditional healthcare, and technological innovation is charting a course for a more connected, efficient, and patient-centered medical experience. Healthcare institutions that embrace this shift will be better equipped to meet the challenges and opportunities of the coming decade. As healthcare becomes more integrated with digital advances, the future of patient care will be defined by seamless, personalized, and accessible medical experiences.
FAQ
Telemedicine offers improved accessibility to healthcare, reduced patient travel time, and increased convenience. It facilitates continuity of care, especially for those in remote areas.
Traditional healthcare involves in-person visits, physical examinations, and treatments, whereas telemedicine utilizes digital platforms to provide remote healthcare services.
Telemedicine can be as effective for many consultations, particularly for follow-ups and managing chronic conditions, though it cannot replace all in-person care.
Challenges include technological barriers, privacy concerns, varying levels of internet access, and the need for regulatory compliance.
Security varies by platform, but they must comply with standards like HIPAA to ensure patient data protection. Users should verify platform security measures.
Telemedicine complements traditional healthcare but may not replace it completely due to the need for physical examinations in certain medical situations.
Technology is revolutionizing healthcare through advancements like telemedicine, AI diagnostics, electronic health records, and no-code development platforms.
No-code platforms like AppMaster enable healthcare providers to create custom applications for patient management, data handling, and telemedicine without extensive programming knowledge.
Legal considerations include compliance with regulations like HIPAA, data protection laws, and obtaining licensure to practice medicine across different regions.
Traditional healthcare can incorporate digital solutions, enhance remote monitoring capabilities, and integrate telemedicine to meet evolving patient expectations.
The future of telemedicine includes greater integration with AI, improved patient engagement, expanded services, and enhanced accessibility worldwide.